Abstract
Introduction: Prone positioning (PP) is beneficial in acute respiratory distress syndrome (ARDS) patients with orotracheal intubated (OTI) patient, however further studies are needed for awake patients with ARDS. We aim to evaluate the relationship between the duration and number of PP and the need for invasive mechanical ventilation (IMV) in awake patients with COVID-19 related ARDS (C-ARDS).
Methods: This is an observational, single-centred, and retrospective study of 32 patients underwent invasive mechanical ventilation (IMV) and matched 33 non-IMV patients with C-ARDS receiving HFNC (high flow nasal cannula). Independent variables such as total number and duration of PP, clinical features, and patient characteristics were obtained. Logistic regression models were used to investigate variables associated with IMV need. Subsequently, models were adjusted for ROX index, APACHE II and SOFA scores, and LOS (length of stay).
Results: The SOFA score, ROX index at 4 h, and LOS differed between groups. PaO2, SpO2, respiratory rate (RR) and ROX index of all patients improved after the first prone position (t = -6,93, p < ,001; t = -7,30, p < ,001; t = 5,35, p < ,001; t = 6,02, p < ,001; respectively). Diagnostic decision-making features of PP number (AUC = 0,690) and PP duration (AUC = 0,723) in predicting the need for IMV were examined with the ROC curve. We found that total number of prone position (aOR: 0,70; [CI %95: 0,51 - 0,96]; p = 0,026) and duration of prone position (aOR: 0,95; [CI %95: 0,92 - 0,99]; p = 0,22) are associated with decreased risk of undergoing IMV.
Conclusion: IMV need is negatively correlated with duration and total number of PP in the awake patients with C-ARDS receiving HFNC, even after adjusting for possible confounding factors. To generalise these results, additional studies that are multi-centred and with a larger sample sizes are needed.
Keywords: acute respiratory distress syndrome, COVID-19, mechanical ventilation, prone position, high flow nasal cannula
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) primarily affects respiratory system and may lead to acute respiratory distress syndrome (ARDS). With the PROSEVA study, prone positioning has become one of the armamentarium of intensive care unit (ICU) specialists, especially dealing with moderate and severe ARDS patients who require mechanical ventilation (1,2). One other tool, high flow nasal cannula (HFNC), can reduce the need for invasive mechanical ventilation (IMV) and improve oxygenation compared to standard oxygen therapy (3). HFNC treatment may further provide beneficial results in both mild and mild-to-moderate COVID-19 related ARDS (C-ARDS) and even in some moderate-severe patients (4).
The need for IMV and mortality rate increased throughout the pandemic. The administration of awake prone position has become widespread among ICU settings because of insufficient amount of the mechanical ventilators and possible adverse effects of IMV. PP helps dorsal zones of the pulmonary to contribute respiration and aids the homogeneous distribution of ventilation, therefore, improves the compliance and the ventilation to perfusion rate (V/P). Furthermore, PP is associated with higher oxygenation level and decreased mortality rate in orotracheal intubated (OTI) patients with non-COVID-19 related ARDS (non-C-ARDS) (1). The prolonged prone positioning improves oxygenation and reduces mortality in severe ARDS patients who have undergone OTI. However, current studies that include patients undergoing IMV suggest conflicting results regarding the effectiveness of prone position in awake patients (5-7). Although studies have shown that prone positioning increases oxygenation, convincing results have not been achieved in terms of avoiding from OTI and reducing mortality (8).
We considered that C-ARDS patients undergoing HFNC may deteriorate rapidly and may require IMV. We thought that the combined use of prone position and HFNC, which is a treatment strategy used for non-C-ARDS patients not associated with COVID-19, may have a positive effect on the patients’ need for IMV in C-ARDS as well. In addition to this, we want to investigate the association between total duration and number of prone positioning and need for IMV.
The primary aim of our study is to evaluate the relationship between the duration and number of prone positioning and the need for IMV in awake patients diagnosed with C-ARDS. The secondary goals are to define the characteristics of the patients, their comorbidities, investigate the influence of prone positioning on several respiratory variables. We determined our hypothesis as “There is an association between time and number of prone and the need for IMV in patients with C-ARDS receiving HFNC.”
Methods and Materials
This study was reported according to the Strengthening the reporting of observational studies in epidemiology (STROBE) Checklist: cross-sectional studies guidelines.
Study design and settings
This study was designed as an observational, retrospective, longitudinal and mono-centric. Patients with COVID-19 admitted to the ICU of the Department of Anaesthesiology and Reanimation in The University of Health Sciences Bakırköy Dr. Sadi Konuk Research and Training Hospital between March 2020 - October 2020 were included.
Procedure
In order to keep SpO2 > 85% of those patients whose requirement of FiO2 ≥ 28% and, HFNC was applied at the range of 60 L/min. The O2 rate of HFNC was regulated between 40 - 80% according to O2 demand. Cooperative, oriented and able to capable of communicating patients were informed about prone positioning, by administering low-dose anxiolytics when needed to anxious patients without sedation, and they were placed in intermittent prone position according to the time they tolerated. The duration of the prone was not predetermined and was maintained according to the tolerance of patients.
After the first prone position applied to the patients, the ROX index (pulse oximetry/fraction of inspired oxygen/respiratory rate), RR, PO2, and SpO2 values were measured. The prone positioning was continued if the patients were considered to be in need of oxygenation. OTI and IMV decision was based on relevant values such as SpO2 < 85%, RR > 35/min, ROX index < 4.88 pulse oximetry/fraction of inspired oxygen/respiratory rate and clinical conditions (increased respiratory distress, increased respiratory effort, or development of additional system failure that impairs haemodynamic).
Clinical procedures also encompassed following: Patients with RR > 35, use of auxiliary respiratory muscles, haemodynamic instability (systolic blood pressure < 90 mm Hg or mean arterial pressure < 60 mm Hg), and altered consciousness was applied OTI in the supine position.
Participants
65 patients with COVID-19 receiving HFNC whose diagnoses were mild/moderate ARDS included in the final analyses in our study.
Inclusion criteria of the study were; i) being diagnosed with mild and moderate ARDS according to the Berlin definition criteria, ii) receiving HFNC, iii) has a diagnose of COVID-19 confirmed by computerised tomography (CT) and/or polymerase chain reaction (PCR) technique. Exclusion criteria of the study were; i) being diagnosed with severe ARDS according to the Berlin definition criteria, ii) being orotracheal intubated at the time of the admission of ICU, iii) receiving OTI in the first six hours of prone positioning, iv) can not tolerate prone positioning, v) receiving sedative medication.
Variables
Sociodemographic data and comorbidities were designated as independent variables. The need to IMV (dichotomous variable) was the outcome variable of this study.
Data sources/measurement
Data of the patients were collected using the Structured Query Language (SQL) of the Metavision/QlinICU Clinical Decision Support Software.
Study size
Due to the nature of the pandemic and controversial results with the prone position in previous studies at the time this study was designed, we did not perform a priori power analysis; therefore, all patients whose data could be reached between the specified dates were included in the study.
Quantitative variables
Sociodemographic data (numerical variable), time until admission to ICU (unit of hour) ROX index and Horowitz rate (PaO2/FiO2) at the time of the admission of ICU, total prone number (discrete numeric variable), and total prone time (unit of hour) were designated as independent co-variables.
Statistical methods
Numerical data with normal distribution were shown as mean (standard deviation), and those without normal distribution were shown as median (interquartile range). In order to compare the variables between the two groups, the test of comparing the means between two independent groups was used for those with normal distribution, and the Mann-Whitney U test was used for those who were not normally distributed. Categorical variables were presented as frequency (percentage), and comparisons between groups were made with Chi-Square or Fischer’s exact test, depending on their adequacy. Two regression models in which the need for MV was designed as the response variable were conducted. In the first model, number of prone position; in the second model, duration of prone position were explanatory variables. We entered ROX index, APACHE II and SOFA scores, and LOS to the model as covariables. Descriptive and inferential statistical analysis and visualisation were performed with R (R Core Team [2020]). A value of p < 0.05 was considered statistically significant.
Results
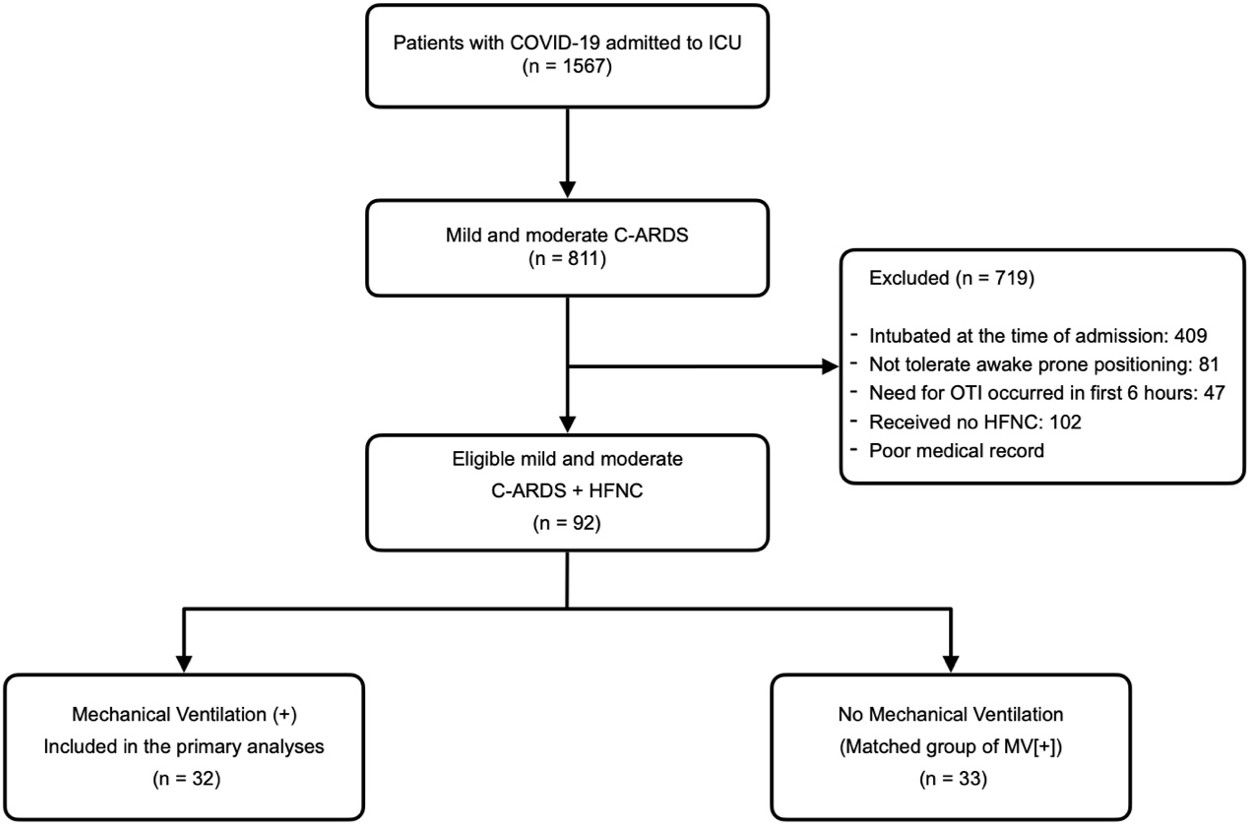
Among 1567 of patients with COVID-19 who admitted to the ICU, we excluded 756 of those not covering mild and moderate ARDS criteria. We included 32 out of 92 potentially eligible patients underwent IMV. Following this, we randomly selected 33 patients as a matched group who didn’t need IMV from the same sample (Figure 1).
The sample of this study is similar to studies involving C-ARDS patients in terms of clinical features, gender, age, and comorbidity (9-11). There were no statistically significant differences between MV (n = 32) and no MV (n = 33) groups in terms of the sociodemographic characteristics, respiratory indicators and comorbidities. However, the SOFA score, the time interval of inpatient unit and ICU admissions, ROX index 4 hours after admission to the ICU differed between these groups. LOS in the ICU also significantly differed between groups, with patients requiring mechanical ventilation experiencing a notably longer LOS (mean = 15.3 days) compared to those not requiring mechanical ventilation (mean = 6.7 days). Detailed descriptive statistics are presented in Table 1.
|
n: Sample size, x: Mean of the sample, SD: Standard deviation, IQR: Interquartile range, C-ARDS: COVID-19 related acute respiratory distress syndrome, HFNC: High flow nasal cannula, BMI: Body mass index, APACHE II: Acute Physiology and Chronic Health Evaluation II, LOS: Length of stay, SOFA: Sepsis related organ failure assessment, ICU: Intensive care unit, RR: Respiratory rate, ROX Index: SpO2/FiO2/RR, Horowitz rate: PaO2/FiO2, pos.: positioning 
The values were obtained at the time of the admission unless otherwise stated. Significant p values are denoted in bold character. |
|||||
| Table 1. Characteristics of the patients with mild or moderate C-ARDS who received HFNC | |||||
|
|
|
|
|
|
|

|

|

|
|||
| Age (years) |
|
|
|
|
|
| BMI (kg/m2) |
|
|
|
|
|
| SOFA |
|
|
|
|
|
| APACHE II |
|
|
|
|
|
| Time Until ICU (hours) |
|
|
|
|
|
| ROX Index |
|
|
|
|
|
| ROX Index at 4h |
|
|
|
|
|
| FiO2 |
|
|
|
|
|
| RR |
|
|
|
|
|
| SpO2 (%) |
|
|
|
|
|
| Horowitz Rate |
|
|
|
|
|
| LOS (days) |
|
|
|
|
|
| Number of PP |
|
|
|
|
|
| Total prone time (hours) |
|
|
|
|
|
|
|
|
|
|
|
|
| Sex, female |
|
|
|
|
|
| Hypertension |
|
|
|
|
|
| Diabetes Mellitus |
|
|
|
|
|
| Coronary Artery Disease |
|
|
|
|
|
| Chronic Kidney Disease |
|
|
|
|
|
| Other Comorbidity |
|
|
|
|
|
|
|
|
|
|||
| No. of Comorbidity |
|
|
|
|
|
PaO2, SpO2, respiratory rate and ROX index of all patients included in final analyses improved statistically significant after first prone position. (Table 2)
|
x: Mean of the sample, SD: Standard deviation, RR: Respiratory rate, ROX Index: SpO2/FiO2/RR 
P values considered statistically significant are denoted in bold |
||||
| Table 2. Oxygenation indicators before and after prone positioning of all patients | ||||
|
|
|
|
|
|

|

|
|||
| PaO2 |
|
|
|
|
| SpO2 |
|
|
|
|
| RR |
|
|
|
|
| ROX Index |
|
|
|
|
Prior to measuring adjusted estimates, each statistically significant independent variable in Table 1 was examined in bi-variable binomial logistic regression models, in which IMV administration was the outcome variable. Increased SOFA score (Odds ratio (OR) = 1,039; [CI %95 = 1,134 - 1,751]; p < ,001), time until ICU admission (OR = 1,015; [CI %95 = 1,004 - 1,025]; p = 0,002), LOS (OR: 1,0101; [CI %95: 1,0049 - 1,015]; p < ,001) were associated with greater risk of need for mechanical ventilation. Increased ROX index after 4 hours of HFNC (OR: 0,816; [CI %95: 0,671 - 0,994]; p = 0,031), number of prone position (OR = 0,767; [CI %95 = 0,643 - 0,914]; p < ,001), and duration of prone position (OR = 0,971; [CI %95 = 0,952 - 0,991]; p < ,001) were associated with decreased risk of undergoing a mechanical ventilation. (Supplementary Table 1)
Diagnostic decision-making features of prone number and duration in predicting the need for IMV were examined with the Receiver Operating Curve (ROC) curve. Sensitivity, specificity, positive predictive and negative predictive values of cut-off values were calculated. (Supplementary Table 2 and Supplementary Table 3) The AUC value of the prone number was 0.690, and of the prone duration was 0.723. (Figure 2)
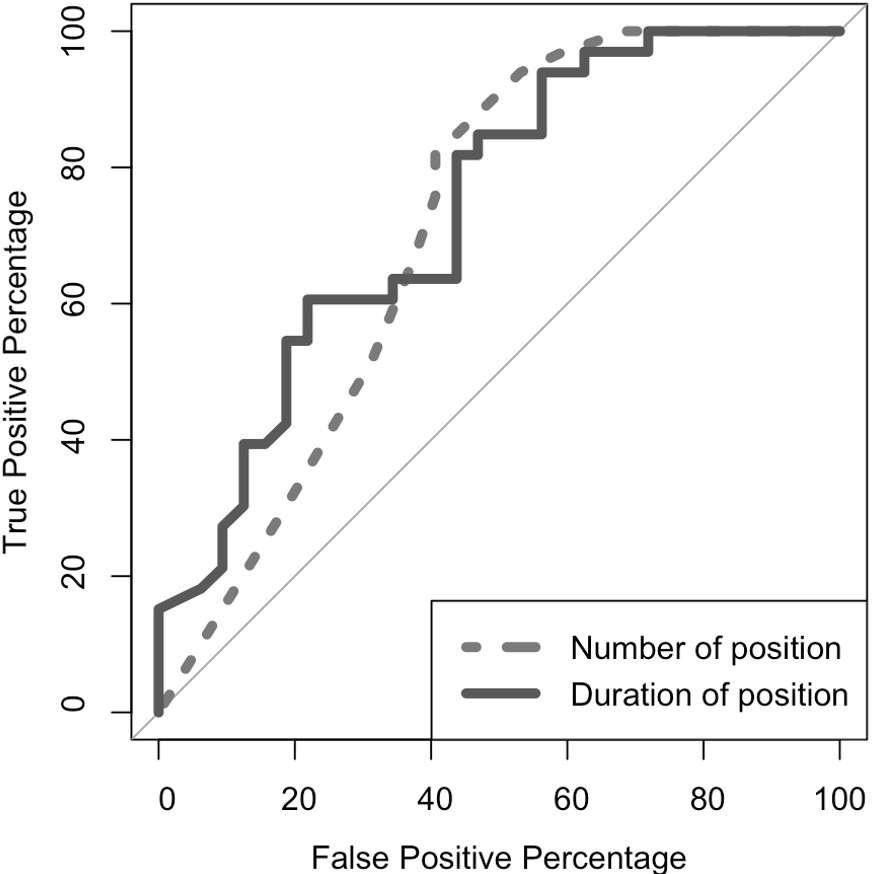
Possible confounders were determined as SOFA score, ROX index, and LOS. After adjusting for other features, higher number of prone position and higher total prone position were associated with smaller risk of mechanical ventilation administration significantly. We confirmed that number of prone position (aOR: 0,70; [CI %95: 0,51 - 0,96]; p = 0,026) and duration of prone position (aOR: 0,95; [CI %95: 0,92 - 0,99]; p = 0,22) are associated with decreased risk of undergoing mechanical ventilation (Table 3).
|
OR: Odds ratio, n: Sample size, CI: Confidence interval, P: probability - p value All multivariable binomial logistic regression analyses were adjusted for possible confounders. P values considered statistically significant are denoted in bold. |
||||||
| Table 3. Multivariable logistic regression models in which need to mechanical ventilation was designed as the response variable (n = 65) | ||||||
| Variable |
|
|
|
|
||
|
|
|
|
|
|||
| Number of prone position |
|
|
|
|
|
|
| Total prone position |
|
|
|
|
|
|
Discussion
Herein, we present a negative correlation between duration and total number of prone position and IMV need of the awake patients with C-ARDS receiving HFNC. The ROX index after 4 hours of the patients required IMV was smaller and the SOFA score of those at the time of the admission were higher compared to of the patients did not require IMV. Additionally, our study shows improved respiratory indicators of all the patients after the first prone position.
The ROX index is an effective marker that can be used for monitoring the course of the disease and the risk of undergoing OTI during the course HFNC treatment. In a similar study, the ratio of oxygen saturation and the ROX index was found to be lower in the IMV group (12). In order to evaluate the success of HFNC in ARDS patients unrelated to COVID-19, a ROX index of less than 4,88 after 12 hours subsequent to HFNC onset may be a guide for OTI (13). Evaluation of the ROX index measured in the first 4 hours after the onset of HFNC in patients with C-ARDS may be helpful to determine the IMV need (14). In our study, the ROX index of the 4th hour of HFNC of the IMV group was smaller than those of the patients did not require IMV. In line with the findings of similar studies, in the present study, we suggest that the ROX index of the 4th hour of HFNC is linked with the need for IMV.
Prone positioning is a treatment strategy used in ARDS patients undergoing OTI with well known physiological effects. These have been investigated in current clinical studies related to the clinical features of extubated patients. A prone position administration is recommended for at least 12 hours a day for ARDS patients who are not associated with COVID-19 and undergoing OTI (15). In patients with moderate to severe C-ARDS, a prone position for 12-16 hours is recommended under IMV (16). With the COVID-19 pandemic, the use of the prone position has begun to increase in awake patients. In a case series of 79 awake patients diagnosed with C-ARDS, HFNC and prone positioning for at least 16 hours were administered and none of these patients, along with an increase in the Horowitz ratio, developed OTI need (17). Therefore, early awake prone positioning together with HFNC can be considered as a treatment modality to prevent IMV in C-ARDS.
Although the physiological effects of the prone position in extubated patients have not been clarified yet, there are many studies showing that it is beneficial in terms of oxygenation. In a research carried out by Sartini et al.(18), it was observed that all patients experienced a decrease in RR both within and prone position and subsequently, and a significant increase in the SpO2 and Horowitz ratio. In another small sample study (n = 10) including patients diagnosed with C-ARDS in Singapore, prone position was applied five times a day for one hour at a regular interval and haemodynamic changes and oxygenation indicators at 0, 30 and 60 minutes improved (19). Another study conducted in Italy in non-intubated patients who remained in the prone position for a minimum of 3 hours experienced increased oxygenation in prone position compared to the supine position (20). Besides, Thompson et al.(21) found that awake C-ARDS patients who remained in the prone position for at least 1 hour and had a SpO2 value above 95% were less in need of IMV. In our study, even a single session of prone positioning increased PaO2, SpO2 and the ROX index and decreased RR.
There are studies in which awake prone positioning is associated with a decrease in mortality rate, as is the need for IMV. In a single-center retrospective study conducted with a series of 105 cases, prone position was associated with a lower rate of OTI and mortality (22). In another retrospective multi-centre observational study, prone position was found to be associated with a lower rate of OTI and mortality in awake patients (23). However, contrary to these findings, a retrospective case-control study (n = 600) reported no significant relationship between awake prone positioning and the need for IMV and mortality. Moreover, it was reported that extubated prone positioning temporarily improved hypoxemia but did not affect the course of the disease (24). In a systematic review and meta-analysis by Li et al.(25) including 29 C-ARDS studies, it was observed that the prone position reduced the need for IMV, but did not have a positive result on mortality. In the present study, a statistically significant relationship was determined between number and duration prone positioning and the reduced need for IMV.
Single prone positioning session is recommended to be at least 120 minutes and for 5-6 hours within a day to increase oxygenation (5). In the present study, considering the time that patients can tolerate in prone positioning, at least 4 hours, cut-off value for each prone positioning of the patients and prone positioning duration cut-off value table were examined. As detecting the real negative event, the need for IMV, is of utmost importance, the cut-off value of the number of prone positioning was determined as 6 times, and the cut-off value of the prone position duration as 64 hours for predicting IMV need considering specificity. Independent of the number of prone positioning and duration, the maximum number and duration of prone positioning that could be tolerated was considered to reduce OTI.
There are some inherent limitations due to the design of the present study. First, the results of our non-prospective study contain inadequacies in terms of generalisability of the results and cause-and-effect relation. In addition, all data were obtained from a single centre, which has been designed solely as an emergency hospital for COVID-19, with adequate mechanical ventilators, physicians and personnel to conduct the daily follow up and treatment of the patients. However, considering that there are many centres that cannot meet these conditions during the pandemic, our findings reveal limitations in terms of generalisability. The outcome variable of the patients, undergoing OTI were left to the clinician’s decision based on patients’ oxygen demand according to SaO2, RR, and ROX index. Leaving the OTI decision to the clinician could be considered as selection bias in our study. In order to reduce the effect of this possible bias as much as possible, we entered ROX index, APACHE II and SOFA scores, and LOS to the logistic models as co-variables.
Conclusion
Our study highlights a negative correlation between the duration and frequency of prone positioning and the need for invasive mechanical ventilation (IMV) in awake COVID-19 associated ARDS (C-ARDS) patients treated with high-flow nasal cannula (HFNC). Key findings indicate that a lower ROX index after 4 hours of HFNC and higher initial SOFA scores correlate with IMV requirement. Prone positioning, applied early and for extended periods, demonstrates significant improvements in oxygenation and potential reductions in IMV needs. Although the ROX index serves as a useful predictor for the necessity of orotracheal intubation during HFNC treatment, the study’s non-prospective, single-center design may limit generalizability. Future multicentric, prospective research is needed to validate these findings and refine treatment protocols across varied clinical environments.
Ethical approval
This study has been approved by the Bakırköy Dr. Sadi Konuk Training and Research Hospital Clinical Research Ethics Committee (approval date: 18.10.2021, number: 2021/490).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159-68. https://doi.org/10.1056/NEJMoa1214103
- Papazian L, Aubron C, Brochard L, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9:69. https://doi.org/10.1186/s13613-019-0540-9
- Rochwerg B, Solo K, Darzi A, et al. Update Alert: Ventilation Techniques and Risk for Transmission of Coronavirus Disease, Including COVID-19. Ann Intern Med. 2020;173:W122. https://doi.org/10.7326/L20-0944
- Li X, Ma X. Acute respiratory failure in COVID-19: is it "typical" ARDS? Crit Care. 2020;24:198. https://doi.org/10.1186/s13054-020-02911-9
- Sodhi K, Chanchalani G. Awake Proning: Current Evidence and Practical Considerations. Indian J Crit Care Med. 2020;24:1236-41. https://doi.org/10.5005/jp-journals-10071-23684
- Jayakumar D, Ramachandran Dnb P, Rabindrarajan Dnb E, Vijayaraghavan Md BKT, Ramakrishnan Ab N, Venkataraman Ab R. Standard Care Versus Awake Prone Position in Adult Nonintubated Patients With Acute Hypoxemic Respiratory Failure Secondary to COVID-19 Infection-A Multicenter Feasibility Randomized Controlled Trial. J Intensive Care Med. 2021;36:918-24. https://doi.org/10.1177/08850666211014480
- Johnson SA, Horton DJ, Fuller MJ, et al. Patient-directed Prone Positioning in Awake Patients with COVID-19 Requiring Hospitalization (PAPR). Ann Am Thorac Soc. 2021;18:1424-6. https://doi.org/10.1513/AnnalsATS.202011-1466RL
- Pavlov I, He H, McNicholas B, et al. Awake Prone Positioning in Non-Intubated Patients With Acute Hypoxemic Respiratory Failure Due to COVID-19. Respir Care. 2022;67:102-14. https://doi.org/10.4187/respcare.09191
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-81. https://doi.org/10.1016/S2213-2600(20)30079-5
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-62. https://doi.org/10.1016/S0140-6736(20)30566-3
- Tu Y, Yang P, Zhou Y, et al. Risk factors for mortality of critically ill patients with COVID-19 receiving invasive ventilation. Int J Med Sci. 2021;18:1198-206. https://doi.org/10.7150/ijms.50039
- Mellado-Artigas R, Mujica LE, Ruiz ML, et al. Predictors of failure with high-flow nasal oxygen therapy in COVID-19 patients with acute respiratory failure: a multicenter observational study. J Intensive Care. 2021;9:23. https://doi.org/10.1186/s40560-021-00538-8
- Roca O, Caralt B, Messika J, et al. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy. Am J Respir Crit Care Med. 2019;199:1368-76. https://doi.org/10.1164/rccm.201803-0589OC
- Zucman N, Mullaert J, Roux D, Roca O, Ricard JD, Contributors. Prediction of outcome of nasal high flow use during COVID-19-related acute hypoxemic respiratory failure. Intensive Care Med. 2020;46:1924-6. https://doi.org/10.1007/s00134-020-06177-1
- Gattinoni L, Taccone P, Carlesso E, Marini JJ. Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am J Respir Crit Care Med. 2013;188:1286-93. https://doi.org/10.1164/rccm.201308-1532CI
- Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020;46:854-87. https://doi.org/10.1007/s00134-020-06022-5
- Xu Q, Wang T, Qin X, Jie Y, Zha L, Lu W. Early awake prone position combined with high-flow nasal oxygen therapy in severe COVID-19: a case series. Crit Care. 2020;24:250. https://doi.org/10.1186/s13054-020-02991-7
- Sartini C, Tresoldi M, Scarpellini P, et al. Respiratory Parameters in Patients With COVID-19 After Using Noninvasive Ventilation in the Prone Position Outside the Intensive Care Unit. JAMA. 2020;323:2338-40. https://doi.org/10.1001/jama.2020.7861
- Ng Z, Tay WC, Ho CHB. Awake prone positioning for non-intubated oxygen dependent COVID-19 pneumonia patients. Eur Respir J. 2020;56:2001198. https://doi.org/10.1183/13993003.01198-2020
- Coppo A, Bellani G, Winterton D, et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020;8:765-74. https://doi.org/10.1016/S2213-2600(20)30268-X
- Thompson AE, Ranard BL, Wei Y, Jelic S. Prone Positioning in Awake, Nonintubated Patients With COVID-19 Hypoxemic Respiratory Failure. JAMA Intern Med. 2020;180:1537-9. https://doi.org/10.1001/jamainternmed.2020.3030
- Jagan N, Morrow LE, Walters RW, et al. The POSITIONED Study: Prone Positioning in Nonventilated Coronavirus Disease 2019 Patients-A Retrospective Analysis. Crit Care Explor. 2020;2:e0229. https://doi.org/10.1097/CCE.0000000000000229
- Rosén J, von Oelreich E, Fors D, et al. Awake prone positioning in patients with hypoxemic respiratory failure due to COVID-19: the PROFLO multicenter randomized clinical trial. Crit Care. 2021;25:209. https://doi.org/10.1186/s13054-021-03602-9
- Nauka PC, Chekuri S, Aboodi M, Hope AA, Gong MN, Chen JT. A Case-Control Study of Prone Positioning in Awake and Nonintubated Hospitalized Coronavirus Disease 2019 Patients. Crit Care Explor. 2021;3:e0348. https://doi.org/10.1097/CCE.0000000000000348
- Li J, Luo J, Pavlov I, et al. Awake prone positioning for non-intubated patients with COVID-19-related acute hypoxaemic respiratory failure: a systematic review and meta-analysis. Lancet Respir Med. 2022;10:573-83. https://doi.org/10.1016/S2213-2600(22)00043-1
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.