Abstract
Objective
The number of oncological patients whose life expectancy has been prolonged thanks to the developments in diagnosis and treatment modalities in the intensive care unit (ICU) is increasing. One of the most common reasons for ethics committee consultation is that patients and their families demand unnecessary restraint from doctors. Although clinical criteria are used to decide whether the applied treatment is useless, it is not sufficient alone to overcome the problems in this regard. The first aim of this study is to draw attention to the futil therapy applied in patients with terminal malignancies in our country and to help determine the necessary strategies to reduce the futility rate. The second purpose is to determine the cost of the futil therapy applied in the intensive care to the health system.
Materials and Methods
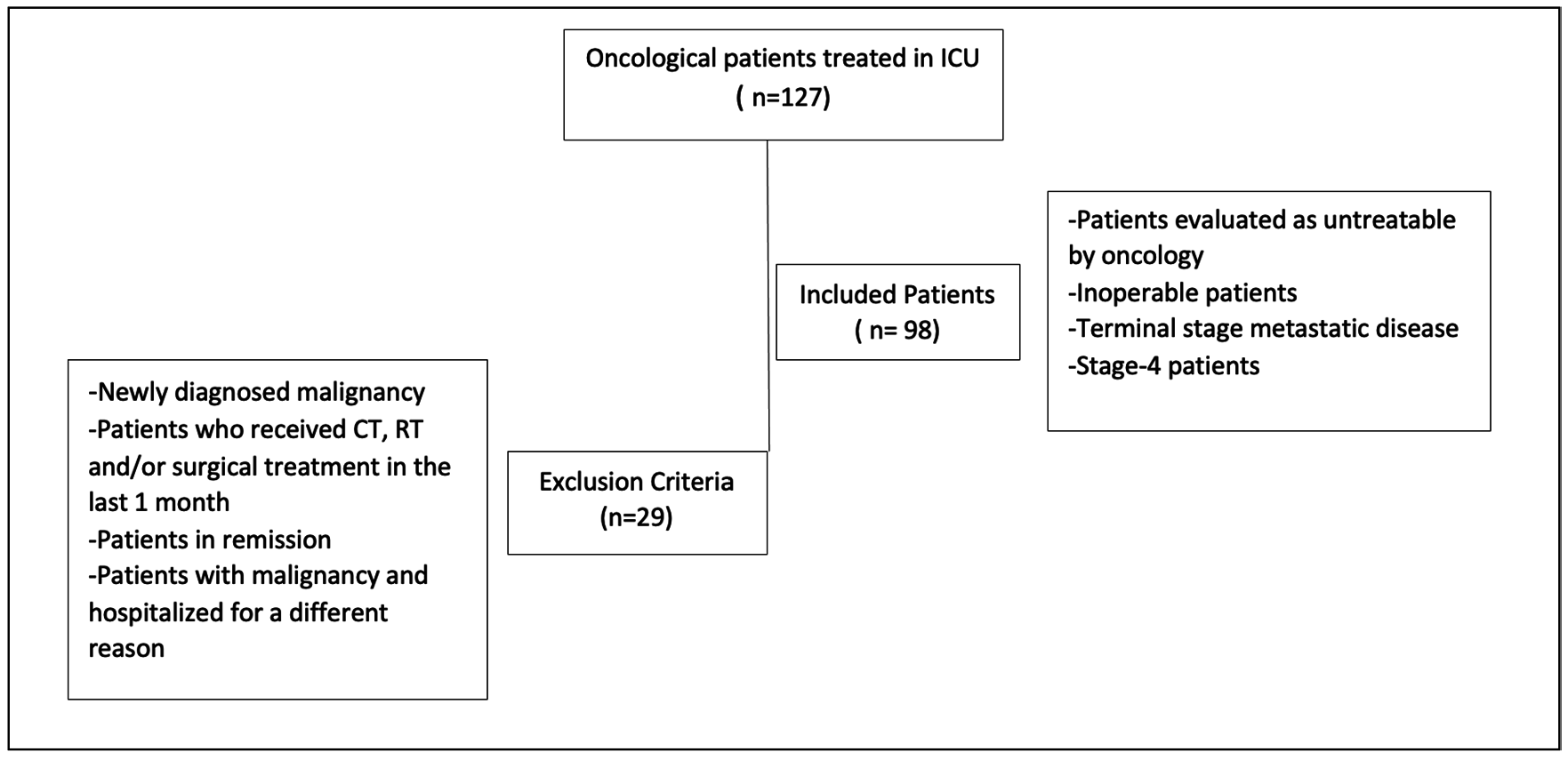
The data of 127 patients with malignancy who were followed up in the ICU between 01 December 2020 and 31 December 2021 were analyzed retrospectively. Stage-4 patients aged 18 years or older with a diagnosis of malignancy, who were recommended palliative treatment by oncologists, and with inoperable, terminal stage, metastatic malignancy were considered as patients who received futile treatment and were included in this study.
Results
Futil treatment was observed in 98 of 127 oncological patients treated in the ICU, and the mortality rate was 86.73% (n=85) in these patients.The cost of futile treatment to the health system was 1.071 intensive care days and $187,907.4 for these patients, who had a high mortality rate, during their stay in the ICU.
Conclusion
With the relevant legal regulations to be made, the evaluation of terminal stage oncological patients by the ethics consultants and the determination of care protocols, and the opening of intermediary ICUs, it can be ensured that patients will have more qualified lifetime.
Keywords: Cost-effective, intensive care, futility, malignancy
Introduction
Intensive care units (ICUs) are medical units with advanced technology, advanced life support, are fully equipped, and are high cost, where doctors, nurses, and allied health personnel serve. Patient admission to the ICU was based on clinical and physiological criteria (1).
The number of oncological patients whose life expectancy has been prolonged because of developments in diagnosis and treatment modalities in the ICU is increasing daily. Indications for admission to the ICU in this patient group often include reasons such as postoperative period, respiratory failure, infection, and sepsis (2).
Although there are scoring systems, such as acute physiologic, chronic health evaluation (APACHE), and simplified acute physiology score, that predict the survival of patients admitted to the ICU, there is still no specific scoring system that predicts the survival of oncologic patients in the ICU. While clinical conditions, such as disease stage, treatments, developing organ failure, mechanical ventilator, and vasopressor, support determine life expectancy in ICU in oncological patients (2). The Eastern Cooperative Oncology Group performance score and karnofsky performance status score (Table 1), which are prevalently used to determine the functional status of patients, also play a role in the treatment and palliative care plan. In addition, studies using these scoring systems have revealed that poor performance status is associated with mortality (3, 4).
| Table 1. Karnofsky performance scoring | ||
|
Progression |
Criteria |
Score (%) |
|
Able to carry on normal activity and to work; no special care needed
|
Normal no complaints; no evidence of disease |
100 |
|
Able to carry on normal activity; minor signs or symptoms of disease |
90 |
|
|
Normal activity with effort; some signs or symptoms of disease |
80 |
|
|
Unable to work; able to live at home and care for most personal needs; varying amount of assistance needed |
Cares for self; unable to carry on normal activity or to do active work |
70 |
|
Requires occasional assistance, but is able to car efor most of his personal needs. |
60 |
|
|
Requires considerable assistance and frequent medical care. |
50 |
|
|
Unable to care for self; requires equivalent of institutional or hospital care; disease may be progressing rapidly |
Disabled; requires special care and assistance |
40 |
|
Severely disabled; hospital admission is indicated although death not imminent |
30 |
|
|
Very sick; hospital admission necessary; active supportive treatment necessary. |
20 |
|
|
Moribund; fatal processes progressing rapidly |
10 |
|
|
Dead |
0 |
|
The willingness of patients and their families to ask for treatment that physicians consider futile is one of the most common reasons for ethics committee consultations (5). Although clinical criteria, such as the inability of the treatment to achieve the goal, imminent death, and the inability of the patient to survive outside of the ICU, are used to decide whether the applied treatment is futile, it is not sufficient alone in overcoming the problems within this regard (6). Hence, in some countries, conflicts between the patient, patient’s family, and physicians have been averted by legal regulations. However, in many countries worldwide, futile treatment has not been fully elucidated. Within the framework of the traditions, customs, and religious beliefs of the societies, the relatives of the patients want their patients to be given full support until the last moment (7). Meanwhile, in our country, due to their legal responsibilities, intensive care specialists cannot refuse patients who require supportive treatment. To prevent patients and their relatives from suffering from the problems experienced, follow-up and treatment continued in the ICU; thereby, the futile treatment rate increased, and the rational use of ICU beds was avoided.
The primary objective of this study was to remark on futile treatment implemented in patients with terminal malignancies in our country and to help determine the necessary strategies to reduce the futility rate. The second objective is to determine the cost of futile treatment implemented in the ICU to the health system.
Materials and Methods
In our study, the data of malignant patients followed in Level 3 ICU between December 01, 2020 and December 01, 2021 were retrospectively reviewed. Stage 4 patients aged 18 years and older, diagnosed with malignancy, who received palliative treatment recommended by oncologists, with inoperable, terminal stage, metastatic malignancy were considered to be patients receiving futile treatment and were included in the present study (Figure 1). Patients with newly diagnosed malignancy, patients who received chemotherapy, radiotherapy, and/or surgical treatment within a month before hospitalization in the ICU, patients who were in remission after malignancy treatment, and patients with malignancy but who were hospitalized in the ICU for reasons independent of malignancy, such as coronavirus disease-2019 (COVID-19), were excluded from this study.
Demographic characteristics of the patients, type of malignancy, APACHE II, sequential organ failure assessment score (SOFA), and Karnofsky performance status score, where and with what symptoms the patients who received futile therapy were admitted to the ICU, and if available in the file records, whether the relatives of the patients requested the treatment were noted. We examined whether patients underwent cardiopulmonary resuscitation (CPR) and intubation without CPR before admission to the ICU. Intubated patients were evaluated in three categories: Intubation before admission, intubation within the first 24 hours, and intubation during follow-up in the ICU. Patients who were intubated before admission were divided into two subgroups: Those with and without CPR. The association between intubation and CPR and mortality was analyzed.
Invasive procedures, such as central vein and artery catheterization, continuous renal replacement therapy (CRRT), tracheostomy, mechanical ventilator (MV) application, radiological imaging, number of consultations ordered for the relevant clinics for treatment and services for transplantation, duration of ICU stay, way the patients exited the ICU was evaluated as discharge to the ward, discharge to the palliative service, and exitus. The 30- and 90-day mortality rates were also analyzed.
The cost calculation was made in accordance with the Healthcare Implementation Communiqué (SUT) payments directive of the TR Ministry of Health, which was mandated on May 01, 2022, considering interventional procedures, other unit consultations, and radiological imaging. Basic patient care practices, such as laboratory, medication, and materials, were not included in the cost calculation.
The present study was approved by the Ethics Committee of University of Health Sciences Turkey, Başakşehir Çam and Sakura City Hospital (no: 49, date: 09/02/2022).
Statistical Analysis
Statistical data were obtained using IBM SPSS Statistics 20 software, and data were expressed as numbers, percentages, and mean ± standard deviation.
Results
In this study, 29 of the 127 oncological patients treated in the ICU were excluded because they were not considered to be receiving futile treatment. Of the 98 patients considered to be receiving futile therapy, 37 (37.76%) were female and 61 (62.24%) were male. The mean age of female patients was 61.97 years, whereas the mean age of male patients was 62.49 years (Table 2).
| Table 2. Demographic characteristics, diagnoses, and scoring of patients | ||
|
Patient sex |
Number of people (%) |
Mean age (min-max) |
|
Female |
37 (37.76%) |
61.97±17.92 (27-93) |
|
Male |
61 (62.24%) |
62.49±13.04 (18-88) |
|
Patient source |
||
|
Lung |
30 (30.61%) |
62.63±12.44 (32-87) |
|
GIS |
21 (21.42%) |
68.14±12.98 (36-88) |
|
Intra-abdominal solid |
9 (9.18%) |
71.33±10.40 (57-93) |
|
Hematology |
9 (9.18%) |
65.44±14.20 (46-89) |
|
Gynecologic |
8 (8.16%) |
57±14.50 (42-89) |
|
Breast |
7 (7.14%) |
51.71±19.6 (27-88) |
|
Suprarenal-renal |
5 (5.10%) |
55.2±14.82 (32-72) |
|
Prostate |
1 (1.02%) |
66 |
|
Brain |
2 (2.04%) |
40.5±31.82 (18-63) |
|
Thyroid |
1 (1.02%) |
29 |
|
Larynx |
1 (1.02%) |
62 |
|
other |
4 (4.08%) |
58±16.49 (40-72) |
|
Patient admission |
||
|
Emergency |
31 (31.63%) |
64.45±12.62 (32-89) |
|
Clinic |
65 (66.33%) |
61.45±16.13 (18-93) |
|
Palliative |
2 (2.04%) |
56.5±9.19 (50-63) |
|
Scoring |
||
|
APACHE- II (mean ± SD) |
24.97±9.81 (10-51) |
|
|
SOFA (mean ± SD) |
10.79±4.86 (2-21) |
|
|
Karnofsky score |
25 (25.51%) |
10 points |
|
|
52 (53.06%) |
20 points |
|
|
21 (21.43%) |
30 points |
| GIS: Gastrointestinal system, APACHE-II: acute physiological and chronic health evaluation-II, SOFA: sequential organ failure assessment, SD: standard deviation | ||
It was determined from the files of eight patients admitted from the emergency department (n=2) and clinical services (n=6) that they and their relatives did not want to continue treatment. Four of these patients underwent CPR. No information on this subject was found in the files of the remaining 90 patients.
The patients were mostly admitted to the ICU from the clinical services, and the most common types of malignancy belonged to the lung and gastrointestinal tract (Table 2). Karnofsky’s performance status score ranged from 10 to 30 points. The main reasons for admission to the ICU were respiratory failure (n=26) and, to a lesser extent, impaired consciousness (n=10), hypotension (n=7), sepsis (n=7), and metabolic disorders (n=9). Among the included patients, 33.6% were admitted to the ICU as intubated, whereas 18.3% were admitted to the ICU after CPR. The reasons for intubation included desaturation, hemoptysis, low Glasgow Coma scale, and hemodynamic instability. Thirty patients admitted to the ICU were intubated within the first 24 hours, and 23 were intubated during the treatment period. In 12 patients, an invasive MV was not required. The ICU stay was 3-28 days in non-intubated patients, while it was 1-82 days in intubated patients (Table 3).
| Table 3. Scoring, MV, number of ICU days, mortality by intubation duration, and CPR | |||||
|
|
Intubated patients before ICU
|
ICU Within first 24 hours Intubated patients (n=30) |
ICU 24 hours- treatment period intubated patients (n=23) |
ICU Non-intubated patients (n=12) |
|
|
|
CPR (+), intubated patients (n=18) |
CPR (-), intubated patients (n=15) |
|
|
|
|
Scoring |
|||||
|
APACHE-2 (mean ± SD) |
32.78±10.23 |
27.87±9.52 |
26.3±9.01 |
17.52±8.63 |
14±7.58 |
|
SOFA (mean ± SD) |
12.95±3.69 |
11.93±3.67 |
12.2±4.51 |
9.48±4.77 |
4.92±4.34 |
|
Karnofsky score/n |
20/3 10/5 |
20/10 10/5 |
30/1 20/25 10/4 |
30/12 20/10 10/1 |
30/8 20/4 |
|
Mean number of days with |
6.22±8.76 (1-29) |
14.33±23.94 (1-82) |
9.57±13.45 (1-57) |
7.04±13.51 (0-61) |
|
|
Mean number of ICU days ± SD (min-max) |
6.22±8.76 (1-29) |
14.33±23.94(1-82) |
10.53±14.8 (1-68) |
12.7±15.38 (2-67) |
11.33±7.94 (3-28) |
|
Mortality |
|||||
|
1st month |
18 (100%) |
12 (80%) |
27 (90%) |
20 (86.96%) |
2 (16.67%) |
|
1st-3rd months |
0 |
3 (20%) |
1 (3.33%) |
3 (13.04%) |
3 (25%) |
|
ICU mortality |
18 (100%) |
15 (100%) |
28 (93.3%) |
23 (100%) |
1 (8.3%) |
| ICU: Intensive care unit, n: number of patients, CPR: cardioplumober resuscitation, APACHE-II: acute physiological and chronic health evaluation-II, SOFA: sequential organ failure assessment, MV: mechanical ventilator, SD: standard deviation | |||||
The mortality rate was 86.73% (n=85) in patients who received futile treatment, and 13 patients had more than one CPR application during their hospitalization. 90.59% (n= 77) of the deaths occurred in the first month, and 8.24% (n=7) occurred within 90 days. Of the patients who received futile therapy, 11.22% (n= 11) were transferred to clinical services and 2.04% (n=2) to the palliative service. The findings showed that four transferred patients died within the first 3 months, and six patients could not be followed up.
In total, 108 central vein catheterizations and 121 arterial cannulations were performed in 98 patients who received futile treatment. Tracheostomy was performed in six patients due to prolonged intubation duration. CRRT support was provided to 11 patients. The radiological imaging methods used and the number of consultations are presented in Table 4.
| Table 4. Special procedures applied to futile therapy patients and their costs | |||
|
The procedure |
Total number (min-max/for a patient) |
Unit price |
Total price |
|
Number of Level 3 ICU days |
1071 (1-82) |
2.476,23 |
2.652.042 |
|
Number of intubation |
53 (0-1) |
44,49 |
2.357 |
|
Number of MV connection |
53 (0-1) |
66,52 |
3.525 |
|
Number of days with MV |
778 (0-82) |
99,68 |
77.551 |
|
Number of intraarterial cannulation |
121 (1-2) |
133,04 |
16.097 |
|
Number of central vein catheterization |
108 (1-3) |
150,04 |
16.204 |
|
Number of CRRT |
11 (0-1) |
179,14 |
1.970 |
|
Number of tracheotomy |
6 (0-1) |
570,15 |
3.420 |
|
Number of direct radiography |
242 (0- 19) |
18,45 |
4.464 |
|
Number of computerised tomography |
5 (0-1) |
149,25 |
746 |
|
Number of magnetic resonance imagining |
1 (0-1) |
176,40 |
176 |
|
Number of CPR |
98 (0-2) |
354,49 |
34.740 |
|
Number of ordered total consultation |
308 (0-26) |
17,27 |
5.319 |
|
Total cost (TL) |
|
|
2.818.611 |
| ICU: Intensive care unit, MV: mechanical ventilator, CRRT: continuous renal replacement therapy, CPR: cardiopulmonary resuscitation, TL: Turkish lira | |||
Health expenses for patients who received futile treatment were calculated according to the TR Ministry of Health SUT Annex-2/C and Annex-2/B, which were in effect on May 01, 2022. It was determined that 2.652.042 TL was spent for 1071 futile ICU days, 83.433 TL for 778 MV follow-up days, which were intubated and followed up with mechanical ventilator, 37.691 TL for invasive procedures, such as arterial and central venous intervention, CCRT, and tracheotomy, 5.386 TL was spent for radiological imaging, and 5.319 TL for consultations (Table 3).
Discussion
In the LST process of patients with oncology at the end of life with high mortality, the religious beliefs and cultural structures of societies are effective in the decision to continue or discontinue treatment. The absence of relevant legal regulations prevents families and physicians from making clear decisions (8). Countries have varying approaches to withdrawal and discontinuation of treatment. However, in our country, legal regulations on this issue are inadequate. Thus, while ICU physicians cannot refuse to accept patients who require supportive treatment, physicians from other branches think and demand that patients in need of palliative care should be followed in ICU due to potential legal problems. In our ICUs, all patient relatives are informed about the process and futile treatment during the terminal period of the disease. However, since it is not legally possible to discontinue treatment, the relatives of patients are not asked whether they want to continue the treatment.
The relatives of patients often want their patients to be given all the support until the last moment, within the framework of the traditions, customs, and religious beliefs of our society. However, we found in the files of eight patients that their relatives wanted the treatment terminated. With the entry into force of the Leonetti law in France, the limits of LST were determined legally. Blythe et al. (7) evaluated post-legal LST in their study among physicians and nurses and reported that the decisions taken by the clear determination of the treatment limits by discussion by the team members involved in the treatment were reliable and applicable to the participants. We found that 77.17% of the patients with malignancy who were followed-up in the ICU at our hospital received futile treatment. All patients underwent an aggressive intensive care follow-up period, and 90.59% died in the first month, whereas 98.83% died within three months. Hence, with legal regulations, it is possible for patients and their relatives to have a say in the continuity of treatment in terminal oncological patients with high mortality. Moreover, the dimensions of futile treatment can be reduced by assessing patients before admission to the ICU with an ethics committee to be established in hospitals.
Advances in fully equipped ICUs and the availability of intensive care physicians are increasing the number of lives saved and the life expectancy of patients. Advanced stage, multiple organ failure, high APACHE-II, and poor performance status adversely affect the prognosis in patients with malignancy followed in the ICU (2). Likewise, in our study, we found that patients with a high APACHE- II score, SOFA score, and Karnofsky performance scale score of ≤30 had a poor prognosis. Kılınç et al. (9), in their study evaluating the prognosis in cancer patients treated in the ICU, also determined the mortality rate as 89.2%. Similarly, we determined the mortality rate as 86.73% in oncological patients receiving futile therapy. We observed that all oncological patients admitted to the ICU after being intubated were mortal. The mortality rate was 93.3% in patients who were intubated within the first 24 hours after hospitalization and 100% in patients who were intubated later on. Although performing CPR in patients with metastatic cancer has contradictory results on survival (10, 11), in our study, all patients (n=21) who underwent CPR after cardiac arrest died within the first month after ICU admission.
Lee et al. (12) from South Korea also revealed in their study that with the well-dying law, families can spend much longer time with the patient, allow doctors to limit life-sustaining treatment, improve the quality of death in the ICU, and the time from DNR to death is longer. It was planned to transfer 17 terminal patients with stable vital parameters in the ICU who did not need supportive treatment to clinical and palliative services so that they could spend more time with their relatives at good quality. However, 62 consultations (min: 1, max: 10) were required to achieve this transfer, and unfortunately, five patients (min: 1, max: 6) died before they could be transferred from the ICU. Undoubtedly, the insufficient number of palliative care units (PCUs) was the most important reason for the observed situation. However, in our study, patients who were followed up in PCUs during the end-of-life period were admitted to the ICU. This suggests the necessity of an intermediary ICU, which is better equipped than palliative services, where less invasive procedures are applied to the patients, is more comfortable, and has a team experienced in terminal malignancies.
The cost of futile treatment during the time these patients with high mortality spent in the ICU was 1071 futile ICU days and 2.652.042 TL. TL was 2.476 TL in one ICU day and 2.575 TL in an ICU day for patients who were intubated and followed up on a ventilator. In addition to providing arterial and vein catheterization to all patients during follow-up, CRRT support was provided to eight patients with hemodynamic instability and renal failure. Percutaneous tracheostomy was performed in six patients due to prolonged intubation duration. The cost of these invasive procedures was 37.691 TL. However, we did not include standard palliative care services, such as nasogastric feeding, pressure ulcer treatment, and antibiotherapy, when calculating the cost. Our aim was to determine the cost resulting from specific procedures performed in the ICU. Huynh et al. determined the cost of 464-day futile treatment of 123 patients followed in the ICU to be roughly 2.6 million dollars (6). Aygencel and Türkoğlu, on the other hand, determined in their study that 83 patients with terminal malignancies cost the healthcare system 581.353,2 TL in 858 ICU days, 677,6 TL per day (13). In the study conducted on oncological patients in Saudi Arabia, the care goals of the patients were determined beforehand, and obligatory recording of the care goals of the patients in the electronic environment was ensured. Ultimately, it was determined that ICU hospitalizations in patients with cancer treated for palliative purposes decreased from 26% to 12%, and some $777.600 was saved annually (14). In our study, the findings showed that as a result of the specific procedures applied to 98 patients who received futile treatment in the ICU, the cost to the health system was approximately 2.818.611 TL ($1=15 TL, $187.907,4) and that if these patients are cared for in the PCU (PCU 927,94 TL/day), approximately 1.824.788 TL ($121.652,5) can be saved. The treatment costs may vary between hospitals and countries. However, it is common worldwide that aggressive treatments and procedures applied in the ICU do not help patients who spend the last days of their lives away from their relatives. This study supports other studies analyzing the economic dimension of futile medical care provided to patients who have no opportunity for treatment (15, 16).
Study Limitations
The limitation of our study is that it was a single-center, retrospective, and planned study during the pandemic. Since most ICU beds were allocated for COVID-19-infected patients during the pandemic, the futility rate in malignant patients seems to be relatively low. Moreover, as patients and their relatives could not be asked for legal reasons regarding whether they demanded treatment continuity, we could not obtain a sufficient number of them in our records.
Conclusion
In conclusion, the rate of futile treatment is increasing due to families’ insistence on advanced treatment, physicians’ belief that this group of patients should end their lives in the ICU, and the lack of legal regulations. With the relevant legal regulations to be established, the evaluation of terminal-stage oncological patients by ethics consultants, the determination of care protocols, and the opening of intermediary ICUs can ensure that patients spend the last period of their lives with less invasive procedures with a more experienced team. Thus, we believe that the cost of futile treatment to the healthcare system may decrease, physicians will be less exposed to the psychological trauma caused by malpractise-compensation cases, and ICU provision may be easier for patients with a higher chance of survival.
Ethics
Authorship Contributions
References
- Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, et al. ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of ınstitutional policies, and further research. Crit Care Med. 2016;44:1553-602.
- Kostakou E, Rovina N, Kyriakopoulou M, Koulouris NG, Koutsoukou A. Critically ill cancer patient in intensive care unit: issues that arise. J Crit Care. 2014;29:817-22.
- De Camargo JD, Delponte V, Costa AZS, da Silva Souza RC. Survival of cancer patients under treatment with the palliative care team in a Brazilian hospital in São Paulo. Can Oncol Nurs J. 2022;32:182-9.
- Van der Zee EN, Noordhuis LM, Epker JL, van Leeuwen N, Wijnhoven BPL, Benoit DD, et al. Assessment of mortality and performance status in critically ill cancer patients: A retrospective cohort study. PLoS One. 2021;16:e0252771.
- Pope TM. Medical Futility. Hester DM, Schonfeld t (editors). Guidance for Healthcare Ethics Committees. Cambridge University Press, Cambridge, UK: 2012. Ch. 12.pp. 88-97.
- Huynh TN, Kleerup EC, Wiley JF, Savitsky TD, Guse D, Garber BJ, et al. The frequency and cost of treatment perceived to be futile in critical care. JAMA Intern Med. 2013;173:1887-94.
- Blythe JA, Kentish-Barnes N, Debue AS, Dohan D, Azoulay E, Covinsky K, et al. An interprofessional process for the limitation of life-sustaining treatments at the end of life in France. J Pain Symptom Manage. 2022;63:160-70.
- Dzeng E, Bein T, Curtis JR. The role of policy and law in shaping the ethics and quality of end-of-life care in intensive care. Intensive Care Med. 2022;48:352-4.
- Kılınç G, Karaduman S, Sungurtekin H. Evaluation of the prognosis of cancer patients treated in intensive care units. J Turk Soc Intens Care. 2022;20:31-7.
- Champigneulle B, Cariou A, Vincent F. Cardiopulmonary resuscitation and benefit to patients with metastatic cancer. JAMA Intern Med. 2016;176:142.
- Schwarze ML, Nabozny MJ, Steffens NM. Cardiopulmonary resuscitation and benefit to patients with metastatic cancer--Reply. JAMA Intern Med. 2016;176:142-3.
- Lee YJ, Ahn S, Cho JY, Park TY, Yun SY, Junghyun K, et al. Change in perception of the quality of death in the intensive care unit by healthcare workers associated with the implementation of the "well-dying law". Intensive Care Med. 2022;48:281-9.
- Aygencel G, Turkoğlu M. General characteristics and costs of terminal stage patients in a medical intensive care unit. J Crit Intensive Care. 2014;5:1-4.
- Salama H, Al Mutairi N, Damlaj M, Alolayan A, Binahmed A, Salama H, et al. Reducing futile acute care services for terminally ill patients with cancer: The dignity project. JCO Oncol Pract. 2021;17:1794-802.
- Carter HE, Winch S, Barnett AG, Parker M, Gallois C, Willmott L, et al. Incidence, duration and cost of futile treatment in end-of-life hospital admissions to three Australian public-sector tertiary hospitals: a retrospective multicentre cohort study. BMJ Open. 2017;7:e017661.
- Schouela N, Kyeremanteng K, Thompson LH, Neilipovitz D, Shamy M, D’Egidio G. Cost of futile ICU care in one Ontario hospital. Inquiry. 2021;58:469580211028577.
Copyright and license
Copyright © 2024 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.






















