Abstract
Objective: Delirium is a common and often misdiagnosed condition associated with increased mortality and cognitive dysfunction in intensive care units. Critical care nurses have a unique opportunity as healthcare providers to assess for and early identify delirium. This study aimed to investigate the knowledge of critical care nurses about delirium care.
Materials and Methods: The study were conducted between April 2022-July 2022 with critical care nurses who had at least one year of experience working in three hospitals. The study data were collected with the “Nurse Characteristic Form” and “Delirium Care Knowledge Questionnaire”.
Results: In total, 253 nurses completed the test. The overall mean score was 10.66±2.29 (possible range 0-16). Correct answers for the subject areas were as follows: (a) 71.1% in symptoms, types, and outcomes; (b) 71.4% in high-risk groups; (c) 81.5% in predisposing and precipitating factors; and (d) 42.7% in assessment and detection. The questions with a high percentage of wrong answers were related to delirium subtypes and assessment. Delirium knowledge scores increased significantly with increasing age and with greater work experience (p<0.05).
Conclusion: The results of this study reveal the need to improve the ability of critical care nurses to accurately identify and assess delirium by using valid tools.
Keywords: critical care, delirium, intensive care unit, knowledge, nursing
Introduction
Delirium is a syndrome characterized by acute alteration in attention, awareness, and cognition, resulting from a medical condition that is cannot be fully explained by a pre-existing neurocognitive disorder (1). While the incidence of delirium in the intensive care unit (ICU) varies between 22-45%, this rate rises to 85% in patients receiving mechanical ventilation (MV) support (2,3).
Delirium in the ICU is associated with important clinical outcomes such as longer ICU stay or MV support, higher mortality, and long-term deterioration in cognitive status after discharge (4,5). This was emphasized by the recent COVID-19 pandemic, which caused an increase in ICU admissions, triggering several risk-factors for delirium (e.g., hypoxia, inflammation, social isolation, and distancing from family) and in effect increased the associated adverse clinical outcomes (6,7). The pandemic underscored the importance of early detection of delirium and controlling it with multi-component treatment methods (pharmacological and non-pharmacological) (6).
Critical care nurses (CCNs) are in a unique position to detect delirium early, identify possible causes, and provide appropriate care, which are critical in improving the quality of care of patients and the patient outcomes (8). Hence, CCNs must put their delirium care knowledge into practice to recognize delirium and provide effective care. However, delirium remains an often missed diagnosis in the ICU, and it has been shown that nurses do not recognize delirium and are not sufficiently familiar with using tools for the assessment of delirium (9-11). The Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU (PADIS) recommend daily routine screening with valid assessment tools for delirium in the ICU (12). However, this recommendation is not put into practice, especially in Turkey, and delirium continues to be a significant problem (13). This lack of implementation of recommendations leads to questions on whether CCNs in Turkey provide appropriate care for patients with delirium. It is crucial for nurses to possess adequate knowledge regarding delirium to provide effective care for these patients. Therefore, this study aimed to investigate the knowledge and awareness of CCNs about delirium care.
Materials and Methods
Design, sample and setting
This cross-sectional research was conducted between April 2022-July 2022 with CCNs working in three training and research hospitals in Bursa, Turkey’s 4th largest city. The ICUs in these hospitals are all secondary and/or tertiary level and provide care for critically ill patients.
At the start of the study, 654 nurses were working in the adult ICUs of the hospitals. No sample selection was performed for the study; we attempted to reach all nurses who met the inclusion criteria. The inclusion criteria were as follows: (a) volunteering to participate in the study, and (b) working in the adult ICUs for at least one year.
Data collection process and instruments
The researchers collected study data through face-to-face surveys conducted at the research centers. In the ICUs where the study was conducted, eligible nurses were informed about the study, and data collection began after obtaining their written and verbal consent. The study data were collected with the “Nurse Characteristic Form” and “Delirium Care Knowledge Questionnaire (DCKQ)”.
Nurse Characteristics Form: This form, prepared by the researchers, included questions about the sociodemographic information of the ICU nurses (age, gender, educational status, etc.) and the characteristics of their work environment (type of ICU unit, work experience, etc.).
Delirium Care Knowledge Questionnaire (DKCQ): This questionnaire was developed by Ho et al. (2021) to determine CCNs’ level of knowledge about delirium care (14). During the development of the tool, available scientific evidence was taken into consideration, including: (a) the “Delirium Care Pathways,” which set the national standards for delirium care in Australia; (b) the Society of Critical Care Medicine’s PADIS guideline; (c) the Scottish Intercollegiate Guidelines Network evidence-based national clinical guidelines in Scotland; and (d) the results of meta-analyses for delirium assessment and detection (14). The DCKQ consists of 16 items designed to measure (a) symptoms, types, and outcomes; (b) high-risk groups; (c) predisposing and precipitating factors; and (d) assessment and detection of delirium care knowledge. The correct answer to each item is scored as 1 point and incorrect or blank answers are scored as 0 points, with the total score ranging from 0 to 16 (14). While most of the items consist of questions with four options, there are also questions with two or five options. In the validity and reliability assessments, the internal consistency and intra-class correlation of the DCKQ were high (0.85 and 0.97, respectively) (14).
Pilot test was conducted with 80 participants (five times the number of items in the DCKQ) to adapt the DCKQ into Turkish and to evaluate its psychometric properties (language and content validity; internal consistency reliability). Firstly, the language validity of the Turkish version of DCKQ (DCKQ-T) was investigated. At this stage, an expert panel was formed by individuals who were proficient in the English language and experienced in the field of ICU and delirium. An expert panel of seven, including two professors (MD), one intensive care specialist (MD), two nursing faculty members (PhD), and two CCNs (with experience of 10 years and more), translated the measurement tool from English to Turkish. By comparing the feedback of the expert panel, care was taken to select the most appropriate expressions in the translation of the measurement tool. The Turkish version of the measurement tool was translated back to English by an independent linguist who did not know about the tool. It was determined that there was a high level of similarity between the translation of the measurement tool from Turkish to English and the original, indicating semantic equivalence.
After ensuring the DCKQ-T’s linguistic validity, the content validity was investigated. An expert panel of five, including two professors (MD), two nursing faculty members (PhD), and one CCN (with over 10 years of experience), were asked to examine the suitability of the items in the DCKQ-T in terms of clarity, scientific content, and measurement and evaluation according to the Davis technique (15). The experts evaluated each item on a four-point scale as (a) the item is appropriate, (b) the item is appropriate but needs minor revision, (c) the item needs major revision, or (d) the item is not appropriate. The number of experts marking (a) and (b) for a particular item was divided by the total number of experts to obtain a content validity index (CVI), which is expected to be 0.80 or higher for a valid item (15). Based on the expert panel’s assessment, the CVI values for the DCKQ-T items ranged from 0.80 to 1.00.
Finally, the internal consistency of the measurement tool was determined by the Kuder-Richardson formula (KR-20), which is commonly used to measure the reliability of binary choice tests (i.e., 0-1 or pass-fail) (16). The KR-20 values range from 0 to 1, and the closer the value is to 1, the better the internal consistency; KR-20 values of 0.70 and above are considered acceptable (16). The internal consistency of the DCKQ-T was found to be high (0.87 for pilot sample, 0.91 for main sample).
After completing the pilot test and ensuring the validity and reliability of the questionnaire, we began measuring nurses’ knowledge level of delirium. Nurses who were included in the pilot test phase were excluded from this phase. The instruments were completed in 10-15 minutes.
Ethical considerations
This study was approved by the Bursa Uludağ University Health Sciences Research and Publication Ethics Committee (Decision no: 2022-03/09). Each investigator obtained the necessary permissions to conduct the study from the management of their respective hospitals. Verbal and written informed consent was obtained from CCNs for participation in the study.
Data analysis
The data were analyzed with Statistical Package for the Social Sciences (SPSS version 23, SPSS Inc, Chicago, USA). The responses were coded as binary variables (1: correct, 0: false). The normal distribution of the data was analyzed using the Shapiro-Wilk test. Descriptive statistics such as frequency, percentage, mean and standard deviation were used to present the data about the characteristics of participating nurses. Two-group comparisons were performed using Pearson’s chi-square or Fisher’s exact test, Mann-Whitney U, or Kruskal-Wallis tests, as appropriate. The level of statistical significance was set as p < 0.05.
Results
Socio-demographic and intensive care characteristics of nurses
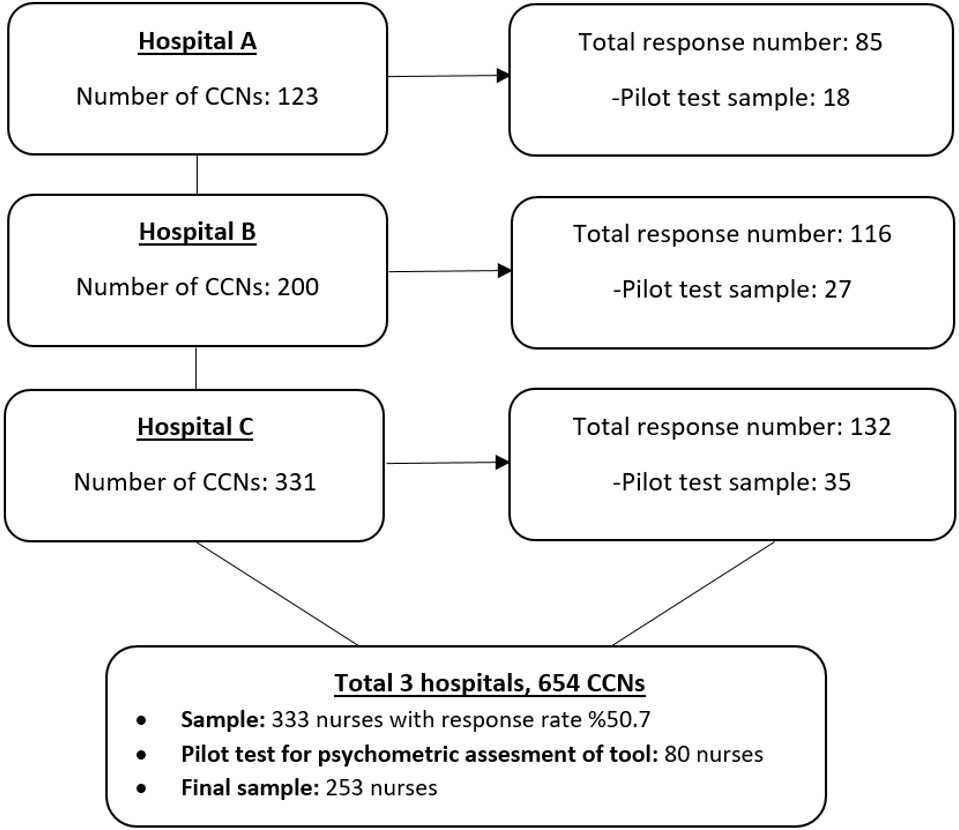
The study sample consisted of a total of 333 nurses and the rate of participation among nurses was 50.9% (Figure 1). A total of 80 nurses who participated in the first pilot test for the psychometric evaluation of the questionnaire were excluded from the sample. As a result, the final sample size was 253 nurses.
The socio-demographic characteristics of the nurses and the characteristics of the ICUs where they work are summarized in Table 1. The mean age of the participants was 31.56±5.41; the majority were female (68.4%) and had a bachelor’s degree (81.8%). The average years of professional experience was 7.61±5.50 while the average years of ICU work experience was 4.83±3.54. The ICUs where the nurses worked were mostly listed as mixed (medical+surgical patients) and internal medicine ICUs (34.4% and 35.2%, respectively). Only 27.3% of the nurses stated that they had received training on delirium care in the last one year, while 65.2% of the trainees did not find this training sufficient and up-to-date. More than half of the nurses (56.5%) stated that they did not evaluate delirium in their ICUs, which was attributed to the complexity of performing cognitive testing (25.4%), lack of hospital-based education (23.9%), and workload (28.0%). Other reasons included the perception that delirium is “normal” since it is common in the ICU (16.7%) and the belief that delirium had no effect on patient outcomes (12.7%). Of the nurses, 40.7% considered the delirium assessment very important.
| M: mean, SD: standard deviation, ICU: Intensive care unit, a: multiple answers. | |
| Table 1. Socio-demographic and ICU characteristics of nurses (N = 253) | |
| Characteristics |
|
| Age (years) |
|
| Age (categorical) | |
| 20-25 years |
|
| 26-30 years |
|
| 31-35 years |
|
| > 35 years |
|
| Gender | |
| Female |
|
| Male |
|
| Education | |
| Associate degree |
|
| Bachelor's degree |
|
| Postgraduate degree |
|
| Type of ICU ward | |
| Mixed/General |
|
| General surgery |
|
| Internal medicine |
|
| Coronary/Cardiology |
|
| Work experience (years) | |
| General |
|
| As an critical care nurse |
|
| General work experience (categorical) | |
| 1-5 years |
|
| 6-10 years |
|
| 11-15 years |
|
| > 15 years |
|
| Critical care nurse work experience (categorical) | |
| 1-3 years |
|
| 4-6 years |
|
| 7-10 years |
|
| > 10 years |
|
| Status of any receiving delirium training (for last 1 year) | |
| Yes |
|
| No |
|
| If ‘yes’, was this training sufficient and up to date? | |
| Yes |
|
| No |
|
| Status of daily delirium assessment in ICU | |
| Yes |
|
| No |
|
| If not, what do you think is/are the reason(s)?a | |
| (a) Workload |
|
| (b) Complexity of conducting cognitive testing |
|
| (c) Considering 'normal' as it is common in ICU |
|
| (d) Believing that it has no effect on patient outcomes |
|
| (e) Absence of a hospital-based training |
|
| The importance of assessing delirium | |
| (a) Very important |
|
| (b) Important |
|
| (c) Neither important or Unimportant |
|
| (d) Unimportant |
|
| (e) Very Unimportant |
|
Delirium care knowledge
The participants’ mean DCKQ-T score was 10.66±2.29. Rates of correct answers in the four sections of the DCQK-T were as follows: (a) 71.1% for symptoms, types, and outcomes, (b) 71.4% for high-risk groups, (c) 81.5% for predisposing and precipitating factors, and (d) 42.7% for assessment and detection (Table 2). When the rates of correct answers given to individual items were examined, the rates were less than 50%, particularly for the item related to delirium subtype and two items about delirium assessment based on the CAM-ICU (45.1%, 32.8%, and 26.9%; Table 2).
| M: mean, SD: standard deviation; CAM-ICU: The Confusion Assessment method for the Intensive Care Unit; PRE-DELIRIC: PREdiction of DELIRium in Intensive Care Unit patients | |||
| Table 2. Scores and correct response rates of all items and sections (N = 253) | |||
| Items |
|
|
|
| Symptoms, types, and outcomes |
|
|
|
| Item 1 (Features of delirium) |
|
||
| Item 2 (Signs and symptoms #1) |
|
||
| Item 7 (Signs and symptoms #2) |
|
||
| Item 8 (Sub-type of delirium) |
|
||
| Item 10 (Delirium outcomes) |
|
||
| High risk groups |
|
|
|
| Item 3 (Risk groups #1) |
|
||
| Item 4 (Risk groups #2) |
|
||
| Item 5 (Risk groups #3) |
|
||
| Predisposing and precipitating factors |
|
|
|
| Item 6 (Cause of delirium) |
|
||
| Item 9 (Risk factors-older patient) |
|
||
| Item 11 (Predisposing factors) |
|
||
| Item 12 (Precipitating factors) |
|
||
| Assessment and detection |
|
|
|
| Item 13 (CAM-ICU assessment #1) |
|
||
| Item 14 (CAM-ICU assessment #2) |
|
||
| Item 15 (PRE-DELIRIC detection #1) |
|
||
| Item 16 (PRE-DELIRIC detection #2) |
|
||
| Total score |
|
|
|
The nurses were compared with respect to their delirium assessment status and delirium training status for items with a high rate of wrong answers (Items 8, 13 and 14; Table 3). The rate of correct answers by those who assess delirium in their ICU and those who do not were similar. This was the same for the comparison between those who received delirium training and those who did not. No significant differences were found in the chi-square analyses (p>0.05).
|
a: Question about delirium subtypes; b: Questions about CAM-ICU assessment. Significance value: p<0.05 |
|||||||
| Table 3. A comparison of nurses based on their delirium assessment and training status for the questions with a high percentage of wrong answers (N = 253) | |||||||
| Items |
|
|
|||||
|
|
|
|
|
|
|
||
| Item 8a | Correct |
|
|
|
|
|
|
| Incorrect |
|
|
|
|
|||
| Item 13b | Correct |
|
|
|
|
|
|
| Incorrect |
|
|
|
|
|||
| Item 14b | Correct |
|
|
|
|
|
|
| Incorrect |
|
|
|
|
|||
The relationship between nurses’ total DCQK-T scores and their characteristics was also examined (Table 4). As the age of the participants increased, the score of delirium care knowledge increased significantly (p=0.30). The DCQK-T scores were significantly higher with more than 15 years of professional experience than those with 1–5 years, 6-10 years or 11–15 years (p=0.01). Participants with more experience as CCN also scored significantly higher (10.18±2.30 points for 1-3 years, 10.53±2.12 points for 4-6 years, 11.20±2.43 points for 7-10 years, and 12.06±1.90 points for > 10 years; p=0.001).
| ICU: Intensive care unit; a: Kruskal-Wallis H Test; b: Mann Whitney U test; *: significance value (p<0.05). | |||
| Table 4. The relationship between nurses' characteristic variables and questionnaire performance (N = 253) | |||
| Demographic Variables |
|
|
|
| Age | 20-25 years |
|
|
| 26-30 years |
|
||
| 31-35 years |
|
||
| > 35 years |
|
||
| Gender | Male |
|
|
| Female |
|
||
| Education | Associate |
|
|
| Bachelor’s |
|
||
| Post-graduate |
|
||
| Type of ICU ward | Mixed/General |
|
|
| General surgery |
|
||
| Internal medicine |
|
||
| Coronary/Cardiology |
|
||
| Work experience (General) | 1-5 years |
|
|
| 6-10 years |
|
||
| 11-15 years |
|
||
| > 15 years |
|
||
| Work experience (As an critical care nurse) | 1-3 years |
|
|
| 4-6 years |
|
||
| 7-10 years |
|
||
| > 10 years |
|
||
| Previous training | Yes |
|
|
| No |
|
||
| Delirium assessment | Yes |
|
|
| No |
|
||
Discussion
The primary objective of this study was to evaluate the level of knowledge among CCNs about providing appropriate care to patients with delirium. Additionally, potential relationships between CCNs’ knowledge levels and their demographic and professional characteristics were examined. The findings provide valuable information about nurses’ knowledge of delirium care and highlight key areas that need attention to improve education and practice related to delirium for nurses.
The findings of our study revealed that the CCNs had a moderate level of knowledge about delirium care (mean correct response rate = 66.6%). This finding supports previous studies that have shown that healthcare professionals, especially nurses, often have deficiencies in their understanding and implementation of delirium management and assessment (17-20). In addition, increasing years of overall work experience and ICU experience with age were associated with higher delirium care knowledge scores. This linear relationship between work experience and delirium care knowledge has also been highlighted in previous studies (11,17,21). As in many professions, experiences gained during work are an important source of knowledge in nursing (22,23). Nurses with more experience may have a higher level of knowledge about the patient care management due to practical experience and ongoing professional development. We believe that experienced nurses can be key figures in providing continues learning and also mentor colleagues in delirium knowledge and management.
The distribution of the correct responses across the sections of the DCKQ-T highlights variations in knowledge domain mastery. The relatively high rates of correct responses in the symptoms, high-risk groups, predisposing and precipitating factors sections suggest that CCNs may have a more robust understanding of recognizing delirium symptoms, distinguishing high-risk patients, and identifying factors that contribute to delirium risk. On the other hand, low rates of correct responses to questions about delirium subtypes and the assessment and detection of delirium indicate the need for targeted educational interventions in these specific areas. One possible explanation for this finding might be attributed to the lack of a daily standardized delirium evaluation protocol in the ICUs of the study centers. Instead, patients are assessed only when delirium is suspected, which can lead to the detection of cases of hyperactive delirium that are easily identified simply because the patient is agitated (24). Hyperactive patients exhibit characteristic heightened psychomotor behaviors or “positive symptomatology,” ranging from mild agitation to combativeness, or even psychosis (25). Although hyperactive delirium may be more easily recognized, studies have shown that the hypoactive delirium type, which is characterized by decreased psychomotor activity, is generally overlooked because of its “silent” symptoms and is even more common than hyperactive delirium (50–55.6% for the hypoactive type, 11–34.0% for the hyperactive type) (26,27). It is critical that nurses have a high level of awareness of all delirium subtypes because a recent meta-analysis of 20 studies and 26,442 adult ICU patients reported that hypoactive delirium was associated with higher mortality compared to hyperactive and mixed delirium (28). This meta-analysis also showed that hypoactive delirium was missed in two-thirds of adult ICU patients. Among the ICU healthcare team, nurses are those who spend the most time with ICU patients during continuous monitoring and care (29). Therefore, they are in a key position in helping to identify patients at risk of delirium, detecting acute cognitive changes in the patient, and applying necessary preventive interventions. With appropriate training given to nurses and on-site practices, hypoactive delirium cases can be prevented from being overlooked, and thus, mortality can be reduced with the correct diagnosis.
The fact that the rate of correct answers to items 8, 13 and 14 was similar among the nurses who reported that they received or did not receive delirium training highlights the inadequacy of the training provided and the urgency of the need for more training. The low level of knowledge about assessment, especially among nurses who reported that they performed delirium assessment is striking. We believe that this may lead to misdiagnosis due to incomplete or incorrect assessment, reduce the accuracy of assessments and lead to high false positive and incomplete assessment rates. In light of these results, it is important to emphasize the necessity of up-to-date and continuing training to be provided by hospital management. To eliminate the lack of knowledge about delirium care and increase the number of correctly diagnosed delirium cases, we believe that it would be beneficial to plan institution-specific trainings. Theoretical trainings is a potentially effective strategy for improving nurses’ delirium-related knowledge and their ability to recognize and manage delirium (30). However, the effectiveness of theoretical training may decrease or disappear over time. Therefore, it may be more effective to use various approaches in combination with theoretical training. A quasi-experimental study found that multi-modal delirium training (online didactics with video simulation and 1:1 bedside coaching) provided to nurses increased their knowledge and confidence in performing delirium assessment (31). Another study examined the impact of an interactive e-learning program comprising four sections on preventing, diagnosing, screening, and treating delirium for CCNs (32). The intervention group demonstrated significantly higher mean scores in delirium recognition skills compared to the control group.
The findings of our study indicated that more efforts are needed to improve the quality of delirium care education. In Turkey, many public and university hospitals under the Ministry of Health carry out “Critical Care Nursing Certificate” programs. In addition, several associations related to ICUs organize Critical Care Nursing courses, and some hospitals offer in-house training and seminars. We believe that further research is necessary to analyze the content of delirium care education offered in these courses or programs. It is important that the content of delirium care training is developed in line with the recommendations in the PADIS guidelines.
Strengths and limitations
One of the strengths of this study is that it was a multi-center study performed in the 4th largest city in Turkey. Another strength is that an up-to-date, evidence-based, valid and reliable assessment tool was used to determine the nurses’ knowledge about delirium care, and the psychometric properties of the Turkish version of this tool were tested and presented to the use of the nursing community in Turkey.
However, this study has some limitations. Since the study was completed with volunteer nurses in the centers, nurses who participated voluntarily may have shown more interest in the subject than those who decided not to participate, which may have led to selection bias. Given the timing of the study, which was conducted shortly after the pandemic, it is possible that the level of knowledge measured may have been lower due to missed training that would normally have been followed, and therefore may not be an adequate representation of the level of knowledge in a ‘normal situation’.
Conclusion
According to the findings of the present study, CCNs show acceptable levels of knowledge on delirium symptoms, outcomes, predisposing and precipitating factors, and high-risk groups. However, there are gaps in knowledge on delirium subtypes and detection. Future studies and training programs should focus on improving the ability of CCNs to accurately detect and assess delirium with current delirium assessment tools.
Ethical approval
This study has been approved by the Bursa Uludağ University Health Sciences Research and Publication Ethics Committee (approval date: 30.03.2022, number: 2022-03/09). Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Wilson JE, Mart MF, Cunningham C, et al. Delirium. Nat Rev Dis Primers. 2020;6:90. https://doi.org/10.1038/s41572-020-00223-4
- Lee G, Roh YS. Knowledge, barriers, and training needs of nurses working in delirium care. Nurs Crit Care. 2023;28:637-44. https://doi.org/10.1111/nicc.12724
- Roh YS. The training needs of Korean intensive care unit nurses regarding delirium. Intensive Crit Care Nurs. 2021;62:102954. https://doi.org/10.1016/j.iccn.2020.102954
- Salluh JI, Wang H, Schneider EB, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350:h2538. https://doi.org/10.1136/bmj.h2538
- Bulic D, Bennett M, Georgousopoulou EN, et al. Cognitive and psychosocial outcomes of mechanically ventilated intensive care patients with and without delirium. Ann Intensive Care. 2020;10:104. https://doi.org/10.1186/s13613-020-00723-2
- Kotfis K, Williams Roberson S, Wilson JE, Dabrowski W, Pun BT, Ely EW. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit Care. 2020;24:176. https://doi.org/10.1186/s13054-020-02882-x
- Ticinesi A, Cerundolo N, Parise A, et al. Delirium in COVID-19: epidemiology and clinical correlations in a large group of patients admitted to an academic hospital. Aging Clin Exp Res. 2020;32:2159-66. https://doi.org/10.1007/s40520-020-01699-6
- Boot R. Delirium: a review of the nurses role in the intensive care unit. Intensive Crit Care Nurs. 2012;28:185-9. https://doi.org/10.1016/j.iccn.2011.11.004
- Özsaban A, Acaroglu R. Delirium assessment in intensive care units: practices and perceptions of Turkish nurses. Nurs Crit Care. 2016;21:271-8. https://doi.org/10.1111/nicc.12127
- Biyabanaki F, Arab M, Dehghan M. Iranian Nurses Perception and Practices for Delirium Assessment in Intensive Care Units. Indian J Crit Care Med. 2020;24:955-9. https://doi.org/10.5005/jp-journals-10071-23502
- Ho MH, Chang HCR, Liu MF, Chen KH, Shen Hsiao ST, Traynor V. Recognizing Intensive Care Unit Delirium: Are Critical Care Nurses Ready? J Nurs Res. 2022;30:e214. https://doi.org/10.1097/jnr.0000000000000487
- Devlin JW, Skrobik Y, Gélinas C, et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit Care Med. 2018;46:e825-e873. https://doi.org/10.1097/ccm.0000000000003299
- Erbay Dalli Ö, Akça Doğan D, Bayram R, Pehlivan S, Yildiz H. Practices of the ABCDEF care bundle in intensive care units as reported by nurses: A cross-sectional study from Turkey. Nurs Crit Care. 2024;29:974-86. https://doi.org/10.1111/nicc.12963
- Ho MH, Traynor V, Chen KH, Montayre J, Lin YK, Chang HR. Delirium care knowledge in critical care nurses: A multiple-choice question-based quiz. Nurs Crit Care. 2021;26:190-200. https://doi.org/10.1111/nicc.12608
- Davis LL. Instrument review: Getting the most from a panel of experts. Appl Nurs Res. 1992;5:194-7. https://doi.org/10.1016/S0897-1897(05)80008-4
- Ekolu S, Quainoo H. Reliability of assessments in engineering education using Cronbach’s alpha, KR and split-half methods. Glob J Eng Educ. 2019;21:24-9.
- Rowley-Conwy G. Critical care nurses' knowledge and practice of delirium assessment. Br J Nurs. 2017;26:412-7. https://doi.org/10.12968/bjon.2017.26.7.412
- Zhou W, Zheng Q, Huang M, et al. Knowledge, attitude, and practice toward delirium and subtype assessment among Chinese clinical nurses and determinant factors: A multicentre cross-section study. Front Psychiatry. 2023;13:1017283. https://doi.org/10.3389/fpsyt.2022.1017283
- Awad SA. Critical Care Nurses' Knowledge, Perception and Barriers Regarding Delirium in Adult Critical Care Units. Am J Nurs. 2019;7:193-8.
- Trogrlić Z, Ista E, Ponssen HH, et al. Attitudes, knowledge and practices concerning delirium: a survey among intensive care unit professionals. Nurs Crit Care. 2017;22:133-40. https://doi.org/10.1111/nicc.12239
- Shrestha S, Shrestha S. Knowledge on Intensive Care Delirium among Nurses at Hospital, Nepal. International Journal of Nursing Research and Practice (IJNRP). 2017;4:23-7.
- Skår R. How Nurses Experience Their Work as a Learning Environment. Vocat Learn 2010;3:1-18. https://doi.org/10.1007/s12186-009-9026-5
- Acebedo-Urdiales MS, Medina-Noya JL, Ferré-Grau C. Practical knowledge of experienced nurses in critical care: a qualitative study of their narratives. BMC Med Educ. 2014;14:173. https://doi.org/10.1186/1472-6920-14-173
- Zhou W, Bai X, Yang Y, et al. Revelations of delirium subtype research: A bibliometric analysis of publications in the past twenty years in the field. Asian J Psychiatr. 2023;83:103561. https://doi.org/10.1016/j.ajp.2023.103561
- Menser C, Smith H. Emergence Agitation and Delirium: Considerations for Epidemiology and Routine Monitoring in Pediatric Patients. Local Reg Anesth. 2020;13:73-83. https://doi.org/10.2147/LRA.S181459
- Jayaswal AK, Sampath H, Soohinda G, Dutta S. Delirium in medical intensive care units: Incidence, subtypes, risk factors, and outcome. Indian J Psychiatry. 2019;61:352-8. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_583_18
- Li X, Zhang L, Gong F, Ai Y. Incidence and Risk Factors for Delirium in Older Patients Following Intensive Care Unit Admission: A Prospective Observational Study. J Nurs Res. 2020;28:e101. https://doi.org/10.1097/jnr.0000000000000384
- Krewulak KD, Stelfox HT, Ely EW, Fiest KM. Risk factors and outcomes among delirium subtypes in adult ICUs: A systematic review. J Crit Care. 2020;56:257-64. https://doi.org/10.1016/j.jcrc.2020.01.017
- Papaioannou M, Papastavrou E, Kouta C, Tsangari H, Merkouris A. Investigating nurses' knowledge and attitudes about delirium in older persons: a cross-sectional study. BMC Nurs. 2023;22:10. https://doi.org/10.1186/s12912-022-01158-9
- Byrnes T. Impact of Delirium Education on Medical-Surgical Nurses' Knowledge. J Nurs Care Qual. 2021;36:291-3. https://doi.org/10.1097/NCQ.0000000000000551
- Choi M, DeGennaro R, Blevins C. Multimodal Education Program to Improve Nurses' Knowledge and Confidence on Delirium Recognition in a Surgical-Trauma Intermediate-Care Setting. J Dr Nurs Pract. 2020;13:31-41. https://doi.org/10.1891/2380-9418.JDNP-D-19-00030
- Najafi Ghezeljeh T, Rahnamaei F, Omrani S, Haghani S. The effects of interactive E-learning on delirium recognition ability and delirium-related strain of care among critical care nurses. J Intensive Care Soc. 2022;23:44-52. https://doi.org/10.1177/1751143720972627
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.