Abstract
Objective: This review aims to provide a synopsis of regional analgesic modalities in the intensive care unit (ICU) context and to evaluate existing literature regarding the benefits and limitations of performing these procedures in critically ill patients. Specifically, we review regional techniques in the setting of traumatic rib fractures and extremity fractures, thoracic surgery, major abdominal surgery, and cardiac surgery. We additionally discuss the limitations of clinical practice in performing regional anesthesia in the ICU setting. Overall, the current literature demonstrates promising benefits of regional analgesia in critically ill patients. However, more extensive high-powered studies are needed to determine optimal analgesic strategies in this tenuous population.
Keywords: Regional anesthesia, intensive care unit, acute pain, pain management, post-traumatic pain
Introduction
Pain is pervasive and burdensome for critically ill patients. Approximately 50-70% of patients in intensive care units (ICUs) suffer from pain (1-3) -a figure likely underestimated considering the prevalence of mechanical ventilation, sedation, and delirium in these populations (2, 4, 5). If untreated, pain related to critical illness can evolve into chronic pathologic pain observed in 14-77% of ICU survivors (6, 7). Patients remember pain long after they leave the ICU (8), with many experiencing post-traumatic stress disorder (9) and ICU-acquired opioid dependence (10). Undertreated pain is also linked to higher mortality rates (11), increased sympathetic stress (12), and decreased tissue oxygen tension, which may lead to poor surgical wound healing and infection (13, 14). Consequently, adequate pain control is paramount in the ICU.
Regional techniques are essential to multimodal analgesia in perioperative populations (15). Such techniques offer significant advantages over multimodal pain medications alone, including reduced risk of persistent postoperative pain (16), superior analgesia with lower opioid requirements (17), and fewer side effects with higher patient satisfaction (18). Furthermore, a recent meta-analysis found that regional techniques reduce postoperative neurocognitive dysfunction in major noncardiac surgery (19). Considering the value of regional techniques in perioperative patients, these modalities may represent a promising direction to optimize pain management in critically ill patients, particularly those with post-traumatic or post-surgical presentations.
In this narrative review, we discuss the utility of regional anesthesia for various patient populations in the critical care unit and the challenges faced when performing regional techniques in this high-acuity setting.
Regional Anesthesia for Post-Trauma Patients in the ICU
Trauma represents a significant source of critical illness, making up 46.9% of patients in the ICU, according to a multicenter prevalence study (20). Of these, the most common traumatic injuries were rib fractures at 41.6%, brain injuries at 38.8%, and hemothorax/pneumothorax at 30.8% (20). Most trauma patients report severe pain (21, 22). However, pain management in the setting of acute trauma can be complicated by hemodynamic instability, airway compromise, and neurologic injury. Furthermore, systemic opioids can cause sedation and depression of cardiovascular and respiratory functions (23, 24), which can worsen a patient’s clinical picture and interfere with neurologic exams. As such, regional techniques are especially advantageous in critically ill trauma patients, providing site-specific analgesia with minimal side effects.
Blunt Thoracic Trauma and Rib Fractures
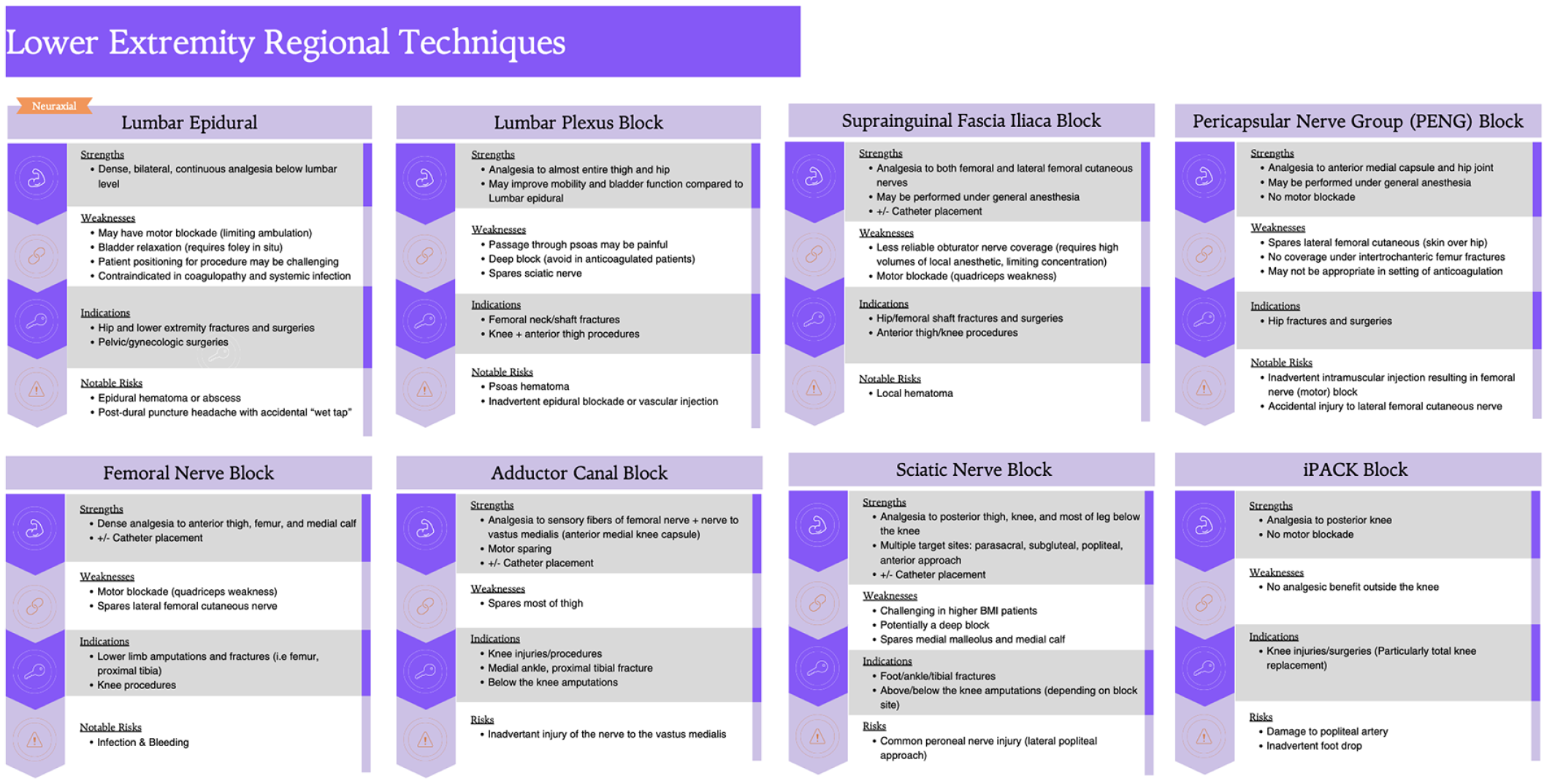
Blunt chest trauma involves injuries ranging from rib fractures, soft tissue contusions, and pneumothoraces (25). Notably, splinting caused by chest wall pain reduces ventilatory effort, which can lead to atelectasis and pneumonia (26). For chest trauma, numerous regional anesthesia techniques can be employed, including thoracic epidural analgesia (TEA), thoracic paravertebral blocks (TPVB), erector spinae plane blocks (ESP), serratus anterior plane blocks (SAP), and intercostal nerve blocks.
In 2016, the Eastern Association for the Surgery of Trauma (EAST) and the Trauma Anesthesiology Society jointly recommended epidurals over non-regional modalities of pain control in blunt thoracic trauma (27). Additionally, two systematic reviews concluded that epidurals provided superior pain relief compared to other modalities in rib fractures (28, 29). However, the idea that epidural analgesia is superior to other regional techniques has been challenged by recent meta-analyses, with both Peek et al. (28) and Duch et al. (30) finding no advantages to epidurals over peripheral blocks in terms of mortality, duration of mechanical ventilation, and pulmonary complications. A meta-analysis of 12 studies found peripheral nerve blocks (TPVBs, intercostal, ESP, and SAP) to have better immediate pain control than conventional analgesics, including epidurals (31). A notable randomized controlled trial (RCT) by McKendy et al. (32) reported increased respiratory complications in patients with multiple rib fractures who received epidurals. However, this observational study has a high potential for selection bias due to the cohort-matched group design determined by the clinician’s decision to place an epidural or not. Particularly in patients with hemodynamic instability or coagulopathy, other regional modalities may be more appropriate and should be considered. An overview of the indications, benefits, and risks of thoracic regional techniques can be found in Figure 1.
Two recent RCTs support the efficacy of paravertebral blocks for improving pulmonary function parameters in rib fractures (33, 34). A scoping review of 37 studies found almost universal improvements in pain and respiratory parameters after ESP blocks in rib fracture patients without complications, even in the setting of anticoagulation and coagulopathy (35). Indeed, RCTs suggest ESP blocks may be as effective as TPVB (36) with lower pain scores compared to intercostal (37) and SAP blocks (38). Independently, the SABRE RCT found clinically meaningful reduction in pain and opioid use with SAP versus standard of care (39). Intercostal blocks with liposomal bupivacaine, while safe, did not improve clinical outcomes (40).
Notably, in geriatric patients, a cohort particularly vulnerable to rib fractures and resultant complications, extensive retrospective studies noted the benefit of early regional intervention to prevent intubation (41) with similar outcomes between TEA and TPVB (42), suggesting further subgroup RCT assessments are needed.
Overall, recent literature on regional techniques in blunt chest trauma remains low quality and heterogeneous, making definitive conclusions regarding the optimal analgesic technique impossible. In fact, by 2023, EAST had changed its previous recommendation for epidurals over systemic modalities due to insufficient evidence of the superiority of epidural or locoregional techniques over other multimodal analgesia. Instead, they suggested providers use their judgment and available resources to provide a multifaceted pain management strategy (43) -a sentiment echoed by Hammal et al. (29) in their updated 2024 systematic review.
Regional Anesthesia for Post-Surgical Patients in the ICU
Around one-third of all critically ill patients worldwide are admitted to surgical ICUs following major elective or emergency surgeries (44, 45). Over half of post-surgical ICU patients report pain at maximal intensity with suboptimal pain control (46). The following section will focus on evidence for the use of regional analgesia for specific subpopulations of post-surgical patients in the ICU.
Extremity Injuries, Surgeries, and Considerations
While traumatic extremity injuries are common, the majority are treated with surgery and will, therefore, be discussed in this section.
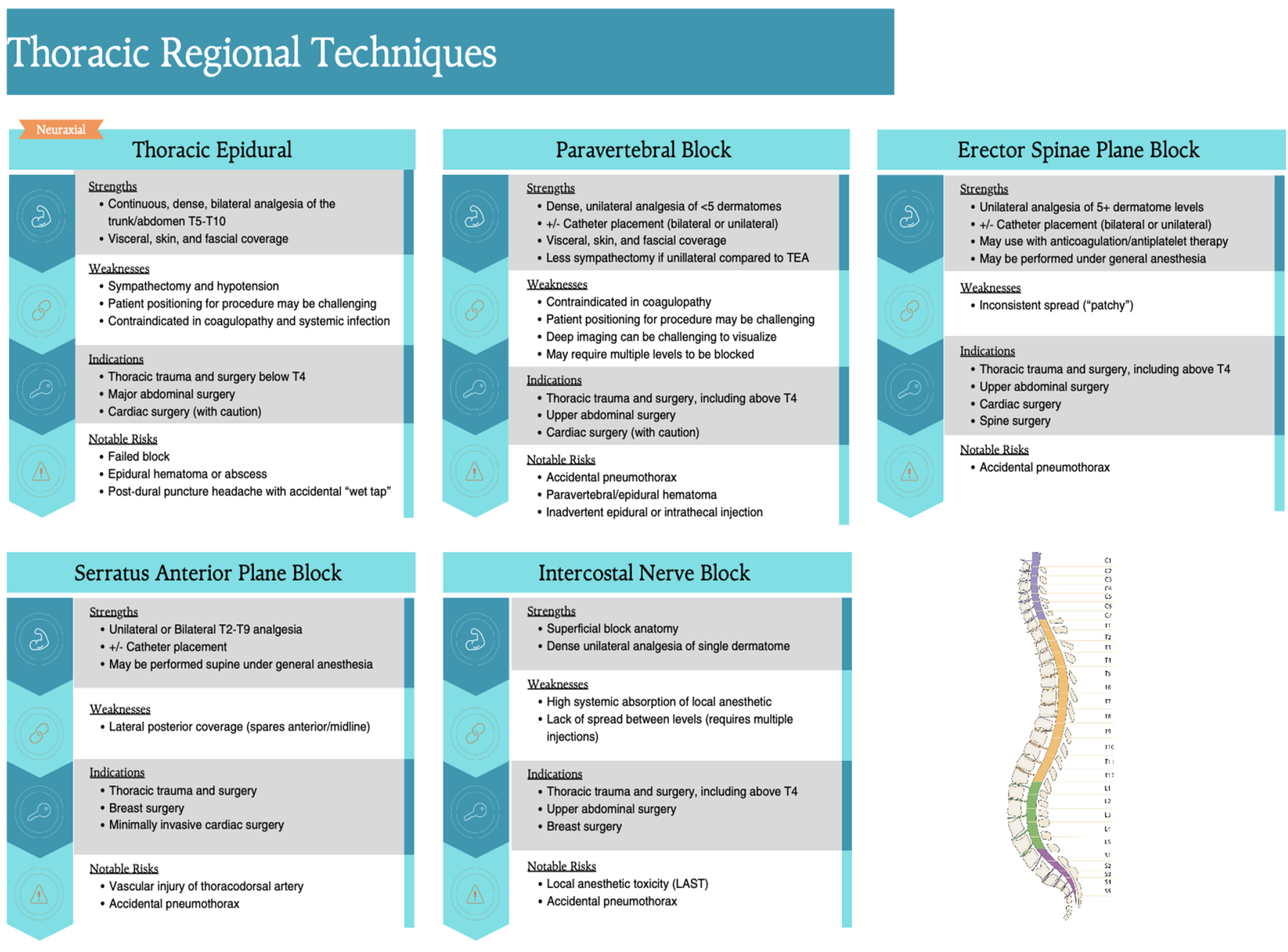
Hip fractures tend to occur in patients who are older, more frail, and have more comorbidities than other trauma patients (47). Lumbar epidural analgesia reduces major adverse cardiac events after hip fracture. The American College of Cardiology/American Heart Association (ACC/AHA) recommended epidural consideration for hip fractures in their 2024 guidelines for perioperative cardiovascular management (48). Peripheral blocks are another alternative, and a Cochrane review of peripheral nerve blocks in hip fractures showed reduced pain scores and confusion in patients receiving regional analgesia (49). The innervation to the hip is complex and involves numerous nerves and their articular branches, including the femoral, obturator, and accessory obturator nerves for the anterior capsule. The posterior joint capsule innervation involves the nerve to the quadratus femoris, sciatic, and superior and inferior gluteal nerves (50). These nerves, in addition to the lateral femoral cutaneous (LFCN), ilioinguinal, iliohypogastric, and posterior femoral cutaneous nerves, contribute to skin innervation over standard surgical incisions for hip fractures. Each nerve can be targeted individually or in combination proximally, like femoral and obturator nerve coverage with a lumbar plexus block. However, newer fascial plane blocks, such as the suprainguinal fascia iliaca and the pericapsular nerve group (PENG), allow multiple nerves to be targeted in a single injection. A multisite RCT found femoral nerve blockade followed by continuous fascia iliaca blocks to provide superior pain scores and walking distances compared to standard systemic therapy in hip fractures (51). Fascia iliaca blockade has been observed to be safe and reliable by a systematic review of 27 RCTs (52). Studies ranging from case series to RCTs support the role of PENG blocks in this fragile patient population (53, 54) which may be superior to femoral and fascia iliaca blocks (55, 56). There is also evidence of benefit when PENG and fascia iliaca blocks are combined (57). Additional blocks with potential efficacy in this patient population include lumbar quadratus lumborum (QL) and ESP blocks (58).
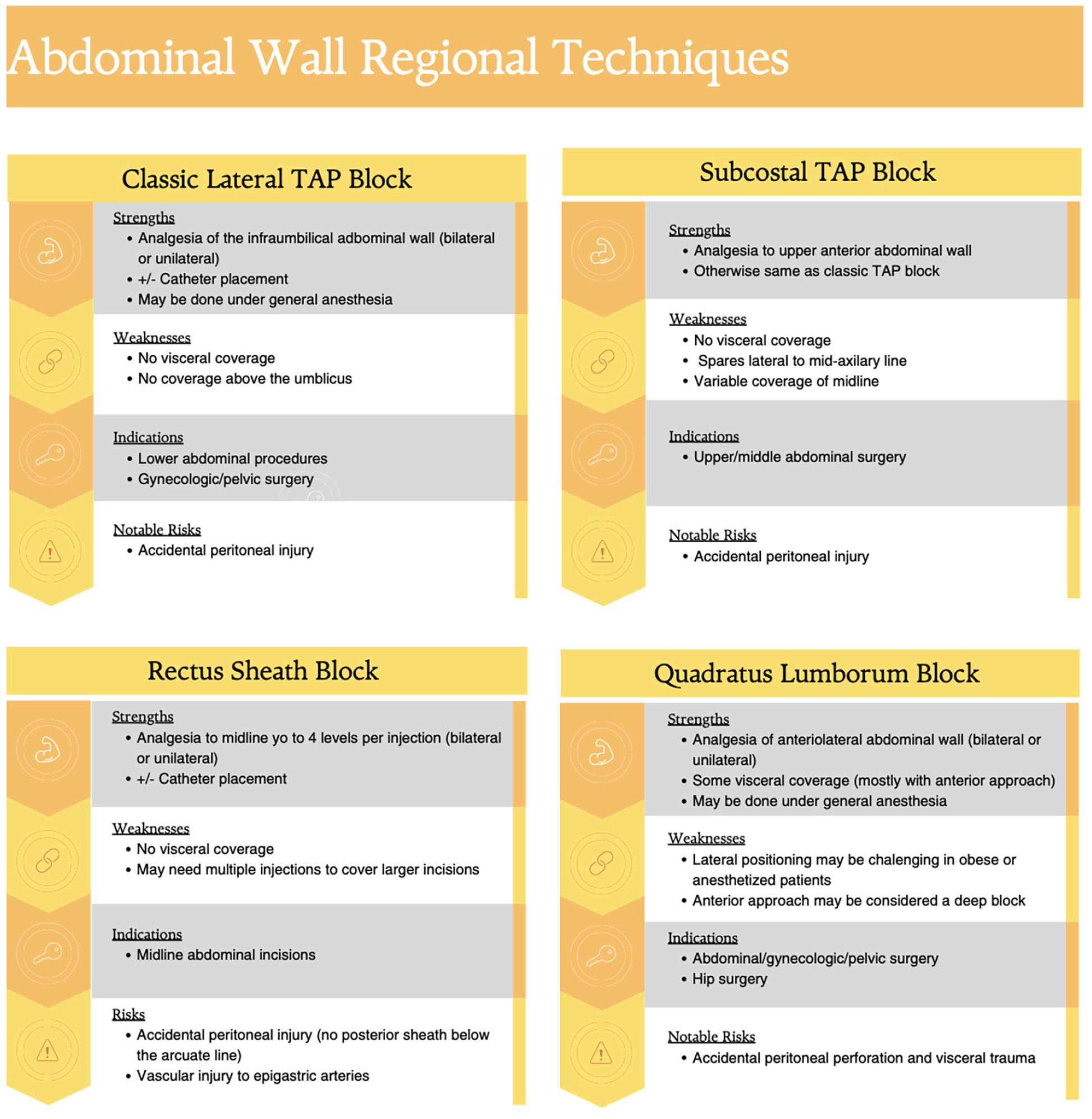
Other types of extremity fractures warrant different regional techniques. Numerous studies demonstrate a reduction in opioid consumption and improved pain scores when regional anesthesia is utilized for extremity fractures (59-61). For clavicle fractures, superficial or intermediate cervical plexus blocks combined with interscalene blockade is a classic combination for both medial and lateral coverage (62). For upper extremity fractures, brachial plexus blocks may be considered, including interscalene, supraclavicular, infraclavicular, costoclavicular, and axillary approaches, as well as individual axillary or suprascapular nerve blocks (63-65). For lower extremity fractures, clinicians can consider femoral, LFCN, adductor canal saphenous, and nerve to the vastus medialis blockade, obturator, genicular, iPACK, parasacral, subgluteal, or popliteal sciatic nerve, and ankle blocks (66-68). The choice of nerve block technique depends largely on the location of trauma, the need for analgesia alone, or the need for surgical-level anesthesia. A summary of regional techniques for upper and lower extremities may be found in Figure 2 and Figure 3, respectively.
When caring for patients with traumatic extremity injuries, the potential for compartment syndrome must be considered. The most common injuries associated with compartment syndrome in descending order are tibial shaft fractures, soft tissue injuries, and distal radius fractures (69). Controversy exists between anesthesiologists and surgeons regarding the potential for regional techniques to delay the diagnosis of this rare but devastating complication by masking one of the earliest clinical signs of compartment syndrome: pain. Unfortunately, the current literature on this subject is not robust and primarily comprises case reports and series. In the last 10 years, there have been two systematic reviews on the subject. Driscoll et al. (70) found that 75% of 34 case reports published since 2009 did not show an increased risk for delayed diagnosis of compartment syndrome following regional anesthesia in orthopedic procedures. Tran et al. (71) found only 6 case reports, 2 of which demonstrated delayed diagnosis of compartment syndrome in the setting of peripheral nerve blockade for long bone fractures. A retrospective study by Cunningham et al. (60) found regional techniques reduced opioid use without incidence of compartment syndrome in tibial plateau fracture. Also notable is a study by Chen et al. (72) in healthy volunteers, which showed regional blocks did decrease ischemic pain but to variable extents, suggesting that regional techniques can be titrated to balance analgesic benefits with the risk of delaying diagnosis. Given the paucity of literature, it is challenging to determine the best analgesic path for patients at risk for compartment syndrome. The European Society of Regional Anaesthesia and Pain Therapy (ESRA) and the American Society of Regional Anesthesia and Pain Medicine (ASRA) 2015 joint committee provided evidence-based advice for pediatric patients focusing on low-dose local anesthetics and infusion rates as well as close monitoring when regional anesthesia is used in high-risk patients (73). Unfortunately, no such recommendations exist in adult populations.
Not all traumatic limb injuries result in fractures. Traumatic amputations have increased globally in recent years (74). Adequate pain control in the setting of amputation is critical due to the risk of phantom limb pain, which is estimated to affect 64% of patients (75) and is thought to be caused by cortical reorganization (76). Regional analgesia may play a fundamental role in mitigating the risk of this debilitating chronic condition (77). A multicentered RCT found that continuous nerve catheters doubled the chance of clinically significant improvement of phantom limb pain (78). However, more studies are needed to elucidate the role of regional anesthesia in this population fully.
Thoracic Surgery
There are many studies on regional anesthesia in thoracic surgery. This review will focus on thoracotomies and esophagectomies to reflect the patient population of the ICU. Thoracic surgery is unique in that pulmonary rather than cardiovascular complications account for most morbidity and mortality (79). A 2017 meta-analysis showed no differences in postoperative pulmonary complications (PPCs) or pain scores between systemic and epidural analgesia or systemic and paravertebral analgesia after esophagectomy. Still, the interpretation is limited by their inclusion of studies that were not high-level RCTs (80). A more stringent 2020 meta-analysis of 2494 patients found low-quality evidence that epidurals reduce the risk of PPCs in patients undergoing major abdominal and thoracic surgery (81). Most recently, a 2024 meta-analysis found a similar reduction of PPCs and better pain reduction associated with epidurals after esophagectomy (82). Other systematic reviews have shown regional techniques can reduce persistent postoperative pain (83) and reduce opioid consumption (84) after thoracic surgeries.
Numerous systematic reviews demonstrate equal analgesic efficacy of paravertebral blocks to epidurals with a lower risk of complications (85-87). Another meta-analysis found TPVBs were superior to ESP for postoperative analgesia after thoracic surgery (88). Even so, two meta-analyses found postoperative pain control benefits from ESP blocks (89, 90). Recent systematic reviews have also shown intercostal blocks to be non-inferior to TPVBs and TEAs (91) and found SAPs to provide effective analgesia in the thoracic surgical population (92-94). Generally, the same variety of regional techniques may be employed for thoracic surgery as for thoracic trauma (as listed in Figure 1), and it is up to the clinician to determine which technique is best on a case-by-case basis.
Patients receiving lung transplants make up a notable population of thoracic surgical patients. TEA is the touchstone for analgesia after lung transplant surgery, though few studies are available in this population. Preoperative TEA is associated with better pain control, lower opioid use, and shorter duration of mechanical ventilation and ICU stay (95). However, TEA must be used cautiously in this population, which may require anticoagulation for extracorporeal membrane oxygenation in the perioperative period (96). Two small studies have also found paravertebral catheters effective (97, 98).
Major Abdominal and Vascular Surgery
TEA is the gold standard for postoperative pain relief after major abdominal surgery (99-101). The 2024 ACC/AHA guidelines recommend thoracic epidurals for major abdominal surgery based on moderate evidence supporting a decreased risk of major adverse cardiovascular events (48).
In open abdominal aortic aneurysm repairs, combined TEA and general anesthesia are associated with reduced mortality, myocardial ischemia, postoperative bowel ischemia, and pulmonary complications (102). The use of TEA in thoraco-abdominal aortic aneurysm repair is associated with better postoperative pain control and lower in-hospital length of stay (103). A Cochrane review of 15 RCTs showed that postoperative epidural analgesia led to better pain management in the first 3 days by Visual Analog Scale scores, earlier tracheal extubation, and lower incidence of myocardial ischemia in this same population (104) However, it is prudent to consider that these studies included primarily trials conducted before 2000, before the availability of endovascular techniques. The impact of TEA on mortality and pulmonary and cardiac complications was not supported by a recent retrospective review of 2,145 patients who underwent aortic aneurysm repair between 2014 and 2016 and found that epidurals were correlated with higher transfusion requirements (105).
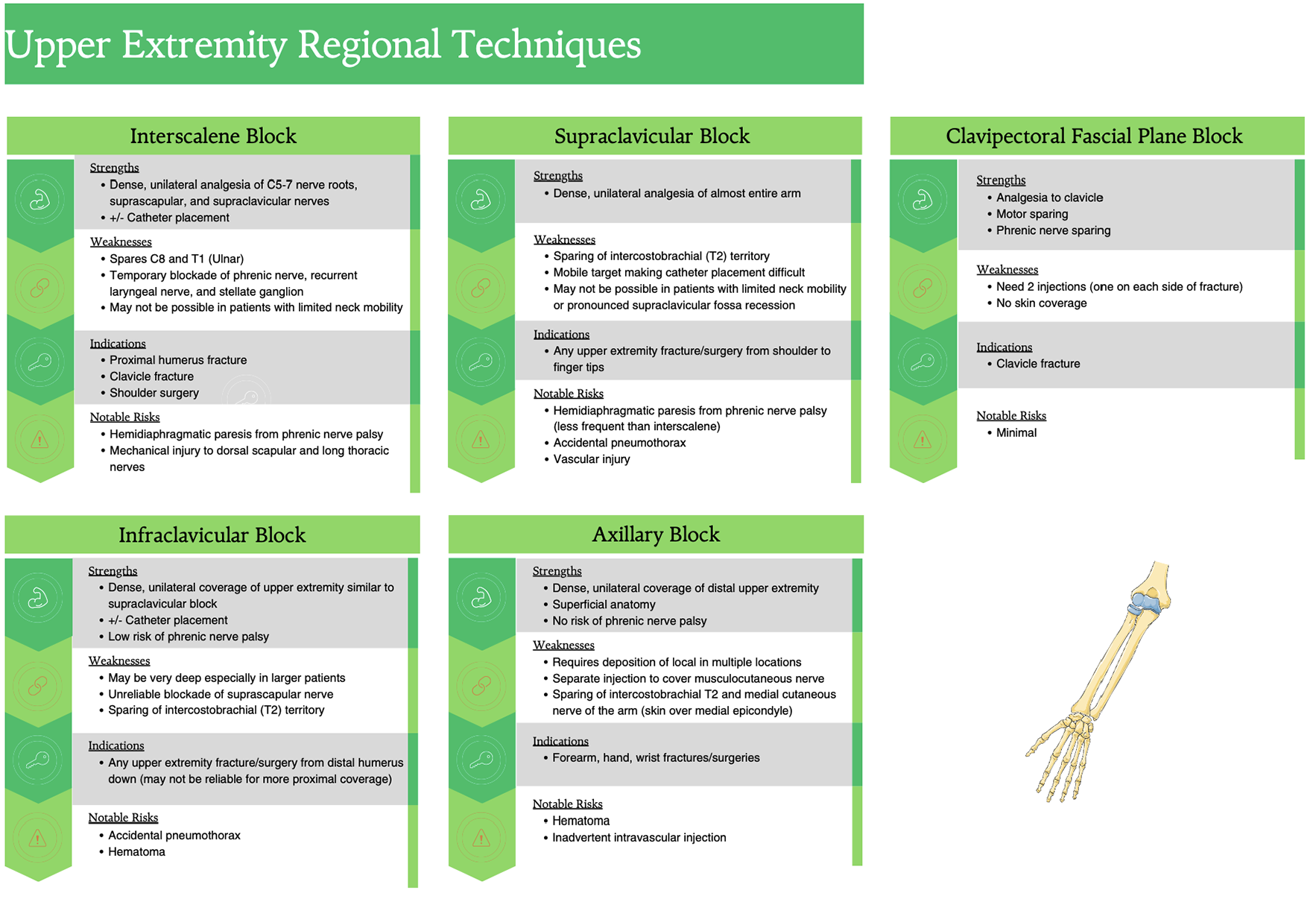
TEA is associated with failure rates as high as 32% (106) and hypotension (107). Additionally, an indwelling catheter is undesirable in a coagulopathic or septic patient, both of which are occasional complications after extensive abdominal surgery. Thus, other effective regional techniques may be considered for major abdominal and vascular surgeries, including paravertebral (108, 109) and erector spinae catheters (110). Paravertebral catheters are likely to be most effective in the case of abdominal aortic aneurysm repair via retroperitoneal approach and have reduced risk of hypotension (108). Fascial plane blocks offer alternatives to TEA. While evidence for fascial plane blocks in the ICU population specifically is lacking, these blocks have been studied extensively in major abdominal surgery, specifically-transversus abdominis plane (TAP), erector spinae plane (ESP), QL, and rectus sheath blocks. Of these, ESP and QL blocks can provide some visceral analgesia due to the spread of local anesthetic to the paravertebral space, but this effect is inconsistent (111). Compared to TEA, studies on fascial plane blocks have demonstrated mixed results. While some studies found TAP blocks to be non-inferior to TEA, others show TEA patients to have lower opioid requirements and pain scores postoperatively (101, 112). Nevertheless, there is consistent evidence that fascial plane blocks effectively decrease the need for postoperative opioids and lower pain scores in comparison to placebo (101, 111, 112). The choice between blocks depends on the surgery and placement of incisions and drains. For example, while rectus sheath blocks are effective for midline incisions, TAP and QL blocks work well for lateral and transverse incisions. A description of abdominal wall regional techniques may be found in Figure 4.
Liver transplant surgery should be considered separately regarding candidacy for regional techniques. Liver transplant recipients have less postoperative pain compared to other major abdominal surgeries, potentially due to denervation of the donor liver, reduced abdominal distention after drainage of ascites, and increased plasma levels of endogenous neuropeptides (113). Even so, liver transplant patients do experience significant postoperative pain and should be provided adequate analgesia. Coagulopathy and thrombocytopenia, often present in these patients, are a contraindication to epidural placement. Additionally, a recent retrospective study of 685 liver transplant patients found preoperative TEA to provide minimal differences in pain scores (Numerical Rating score of 1.4 vs 1.8) compared to patients without TEA (114). However, TEA is an effective mode of pain relief after open liver resection, including for donor liver resection, and has been shown to decrease opioid consumption in the postoperative period (115). Paravertebral catheters and single-shot blocks have also been effective, though pain control is inferior to TEA (115, 116). TAP catheters and blocks are also an effective modality but have not been compared head to head with TEAs or PVBs (115, 116).
Cardiac Surgery
We will briefly mention the utility of regional analgesia in cardiovascular surgical patients as they tend to present to subspecialty ICUs. Patients undergoing open heart surgery frequently require anticoagulation for cardiopulmonary bypass, which makes the use of TEA controversial. A Cochrane review concluded that TEA reduced pain scores by 1 point on a scale of 0 to 10, decreased the length of mechanical ventilation by 2.4 hours, and decreased the rate of myocardial infarction, atrial fibrillation, and respiratory depression at 30 days post-cardiac surgery (117). However, the evidence in this study was of low quality overall, and there was insufficient data to comment on the incidence of epidural hematoma. Based on mathematical modeling, the incidence of spinal injury from epidural hematoma is estimated between 1:150,000 and 1:1,500 for epidurals in conventional cardiac surgery (118). Of note, the 2018 ASRA guidelines state that there is insufficient evidence for an increased risk of epidural hematoma in the setting of cardiopulmonary bypass (119). Meanwhile, paravertebral blocks have been used increasingly for cardiac surgery, particularly in minimally invasive procedures performed via lateral thoracotomy (120). Paravertebral catheters placed perioperatively decrease intraoperative opioid use, reduce nausea and vomiting, and shorten the length of mechanical ventilation with minimal hypotension (121, 122). In this patient population, it is essential to remember that paravertebral blocks are still considered a deep block, which puts them at higher risk in the setting of anticoagulation.
Limitations in Clinical Practice
Sedation
The prevalence of sedation among ICU patients presents a challenge to the performance of regional techniques. Light to moderate sedation, which maintains meaningful contact with the patient, is generally beneficial by providing anxiolysis and increasing patient tolerance of regional nerve blockade (123). However, controversy exists regarding the safety of performing regional blocks on patients under deep sedation or general anesthesia, which obliterates feedback from the patient regarding periprocedural paresthesias and signs or symptoms of local anesthetic toxicity. Many assert that it is necessary for patients to be awake and cooperative enough to communicate when there is pain or paresthesia during a nerve block to protect against neural injury. This concern mainly applies to blocks targeted directly at a nerve versus fascial plane techniques, which are considered safe even under general anesthesia due to the lower risk of nerve damage (124). Indeed, ASRA recommends against regional techniques in heavily sedated or anesthetized patients unless the benefit clearly outweighs the risk (125). Even so, there is little evidence that pain or paresthesia predicts neural injury (126). In fact, regional techniques are routinely used safely in anesthetized pediatric patients. A study by the Pediatric Regional Anesthesia Network of over 100,000 blocks found no incidence of permanent neurologic deficits (127). A prospective study in sedated and mechanically ventilated trauma patients concluded that continuous regional anesthesia seems safe in the setting of heavy sedation-although with 76 patients analyzed, it was underpowered to see significant differences in outcomes (128). As such, the decision to perform regional techniques in heavily sedated patients in the ICU should be considered on a case-by-case basis with careful assessment of the risk-to-benefit ratio. Of note, the 2018 Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Panel within the Society of Critical Care Medicine Congress strengthened their recommendation of light versus deep sedation in the management of critically ill patients, therefore in many cases this obstacle to providing regional anesthesia may lessen (129).
Sepsis and Infection
ICU patients frequently have pre-existing or nosocomial infections (130). Puncture site infection is an absolute contraindication to any regional technique. Systemic infection is often considered a relative contraindication to regional anesthesia due to concerns about seeding infection into fascial planes, nerves, or the neuraxial space, especially in the setting of indwelling catheters. A recent systematic review across various patient populations found that the incidence of infectious complications for central neuraxial blockade was 9/100,000 and 1.8% in peripheral nerve catheters (131). Recent studies show a low incidence of central nervous system infection after neuraxial techniques in patients at risk for or with active bacteremia in the acute perioperative period (132). However, ICU admission is a risk factor for infection of peripheral nerve catheters (133), especially if they are in situ for over 48 hours (134). Factors that may reduce the risk of infection include prophylactic antibiotics (135) and tunneling of catheters (136). The risk of infection must be weighed against the benefits of regional techniques. Any indwelling catheters should be removed as early as is reasonable to minimize colonization while preserving maximal analgesic benefit.
Coagulopathies
Many patients in the ICU experience coagulopathies of various etiologies due to sepsis or trauma (137, 138). Additionally, the use of anticoagulants and antiplatelet medication is expanding. Thus, clinicians must weigh the risks of regional anesthesia in patients susceptible to bleeding. ESRA and ASRA have guidelines for time intervals after cessation of antiplatelet and anticoagulant therapies before performing regional and neuraxial techniques (119, 139). Bleeding complications following peripheral nerve blocks in patients on antiplatelet and anticoagulant medications are rare, estimated to be less than 1% (140). When weighing the risks for hematoma in coagulopathic patients, it is crucial to consider the depth and compressibility of the site for each regional technique. Neuraxial techniques have the highest relative risk followed in descending order of risk by deep blocks such as deep lumbar plexus, proximal sciatic, and infraclavicular blocks, in addition to perivascular blocks such as femoral or axillary blocks, then fascial plane blocks (141). Although controversial, many practitioners feel perineural catheters have a higher risk for bleeding, given they require a larger, blunt tip needle for placement, and there is an additional risk with catheter removal or dislodgement (142).
Hemodynamic Instability
Hemodynamic instability is a common concern in the critically ill, estimated to affect 19% of patients in the ICU (143). The cardiovascular stability of a patient must be considered in the context of regional analgesic techniques. Specifically, neuraxial techniques, such as epidurals and spinals, are associated with hypotension and bradycardia in the setting of sympathetic blockade (144, 145). As such, neuraxial analgesia may be best avoided in patients already at significant risk for hemodynamic compromise or already on vasopressor support. Consideration of shifting from a local anesthetic epidural infusion to solely an opioid infusion, such as fentanyl, may decrease hypotension (146, 147). Even single-sided TVPB may decrease the total local anesthetic spread to the spinal sympathetic chain, lessening the risk of hypotension (85, 87, 108, 148). On the other hand, peripheral nerve blockade may be beneficial in tenuous patients by avoiding the use of sedation medications, which can also compromise cardiovascular stability (149). For example, superficial cervical plexus blockade can facilitate awake central line cannulation (150) and intercostal block may be used for chest tube placement (151).
Conclusion
For patients in the ICU, pain is a prominent concern often associated with long-term consequences. Regional techniques offer targeted analgesia, generally without systemic side effects. From rib fractures and limb fractures to major surgeries, there is a clear benefit to regional analgesia among critically ill patients. However, current literature is insufficient to determine the best technique for optimal pain control in every case. As such, each patient should be evaluated carefully to determine their candidacy for regional analgesia versus systemic pain management alone. Hemodynamic status, infection, level of sedation, and site of surgery or injury are all factors to consider when choosing the best regional modality for each patient.
Ethics
Authorship Contributions
References
- Chanques G, Sebbane M, Barbotte E, Viel E, Eledjam JJ, Jaber S. A prospective study of pain at rest: incidence and characteristics of an unrecognized symptom in surgical and trauma versus medical intensive care unit patients. Anesthesiology. 2007;107:858-60.
- Desbiens NA, Wu AW, Broste SK, Wenger NS, Connors AF Jr, Lynn J, et al. Pain and satisfaction with pain control in seriously ill hospitalized adults: findings from the SUPPORT research investigations. For the SUPPORT investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatmentm. Crit Care Med. 1996;24:1953-61.
- Gélinas C. Management of pain in cardiac surgery ICU patients: have we improved over time? Intensive Crit Care Nurs. 2007;23:298-303.
- Bertolini G, Minelli C, Latronico N, Cattaneo A, Mura G, Melotti RM, et al. The use of analgesic drugs in postoperative patients: the neglected problem of pain control in intensive care units. An observational, prospective, multicenter study in 128 Italian intensive care units. Eur J Clin Pharmacol. 2002;58:73-7.
- Alderson SM, McKechnie SR. Unrecognised, undertreated, pain in ICU—Causes, effects, and how to do better. Open J Nurs. 2013;03:108–13.
- Kemp HI, Laycock H, Costello A, Brett SJ. Chronic pain in critical care survivors: a narrative review. Br J Anaesth. 2019;123:e372-e384.
- Mäkinen OJ, Bäcklund ME, Liisanantti J, Peltomaa M, Karlsson S, Kalliomäki ML. Persistent pain in intensive care survivors: a systematic review. Br J Anaesth. 2020;125:149-58.
- Puntillo KA, Max A, Chaize M, Chanques G, Azoulay E. Patient Recollection of ICU Procedural Pain and Post ICU Burden: The Memory Study. Crit Care Med. 2016;44:1988-95.
- Granja C, Gomes E, Amaro A, Ribeiro O, Jones C, Carneiro A, et al. Understanding posttraumatic stress disorder-related symptoms after critical care: the early illness amnesia hypothesis. Crit Care Med. 2008;36:2801-9.
- Puntillo KA, Naidu R. Chronic pain disorders after critical illness and ICU-acquired opioid dependence: two clinical conundra. Curr Opin Crit Care. 2016;22:506-12.
- Yamashita A, Yamasaki M, Matsuyama H, Amaya F. Risk factors and prognosis of pain events during mechanical ventilation: a retrospective study. J Intensive Care. 2017;5:17.
- Burton AR, Fazalbhoy A, Macefield VG. Sympathetic Responses to Noxious Stimulation of Muscle and Skin. Front Neurol. 2016;7:109.
- Akça O, Melischek M, Scheck T, Hellwagner K, Arkiliç CF, Kurz A, et al. Postoperative pain and subcutaneous oxygen tension. Lancet. 1999;354:41-2.
- Buggy DJ, Doherty WL, Hart EM, Pallett EJ. Postoperative wound oxygen tension with epidural or intravenous analgesia: a prospective, randomized, single-blind clinical trial. Anesthesiology. 2002;97:952-8.
- Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17:131-57.
- Weinstein EJ, Levene JL, Cohen MS, Andreae DA, Chao JY, Johnson M, et al. Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children. Cochrane Database Syst Rev. 2018;4:CD007105.
- Richman JM, Liu SS, Courpas G, Wong R, Rowlingson AJ, McGready J, et al. Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesth Analg. 2006;102:248-57.
- Kumar K, Kirksey MA, Duong S, Wu CL. A Review of Opioid-Sparing Modalities in Perioperative Pain Management: Methods to Decrease Opioid Use Postoperatively. Anesth Analg. 2017;125:1749-60.
- Singh NP, Makkar JK, Borle A, Singh PM. Role of supplemental regional blocks on postoperative neurocognitive dysfunction after major non-cardiac surgeries: a systematic review and meta-analysis of randomized controlled trials. Reg Anesth Pain Med. 2024;49:49-58.
- Michetti CP, Fakhry SM, Brasel K, Martin ND, Teicher EJ, Newcomb A, et al. Trauma ICU Prevalence Project: the diversity of surgical critical care. Trauma Surg Acute Care Open. 2019;4:e000288.
- Kejela S, Seyoum N. Acute pain management in the trauma patient population: are we doing enough? A prospective observational study. J Trauma Inj. 2022;35:151-8.
- Berben SA, Meijs TH, van Dongen RT, van Vugt AB, Vloet LC, Mintjes-de Groot JJ, et al. Pain prevalence and pain relief in trauma patients in the Accident & Emergency department. Injury. 2008;39:578-85.
- Paul AK, Smith CM, Rahmatullah M, Nissapatorn V, Wilairatana P, Spetea M, et al. Opioid Analgesia and Opioid-Induced Adverse Effects: A Review. Pharmaceuticals (Basel). 2021;14:1091.
- Krantz MJ, Palmer RB, Haigney MCP. Cardiovascular Complications of Opioid Use: JACC State-of-the-Art Review. J Am Coll Cardiol. 2021;77:205-23.
- Dogrul BN, Kiliccalan I, Asci ES, Peker SC. Blunt trauma related chest wall and pulmonary injuries: An overview. Chin J Traumatol. 2020;23:125-38.
- May L, Hillermann C, Patil S. Rib fracture management. BJA Educ. 2016 Jan;16(1):26–32.
- Galvagno SM Jr, Smith CE, Varon AJ, Hasenboehler EA, Sultan S, Shaefer G, et al. Pain management for blunt thoracic trauma: A joint practice management guideline from the Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society. J Trauma Acute Care Surg. 2016;81:936-51.
- Peek J, Smeeing DPJ, Hietbrink F, Houwert RM, Marsman M, de Jong MB. Comparison of analgesic interventions for traumatic rib fractures: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2019;45:597-622.
- Hammal F, Chiu C, Kung JY, Bradley N, Dillane D. Pain management for hospitalized patients with rib fractures: A systematic review of randomized clinical trials. J Clin Anesth. 2024;92:111276.
- Duch P, Møller MH. Epidural analgesia in patients with traumatic rib fractures: a systematic review of randomised controlled trials. Acta Anaesthesiol Scand. 2015;59:698-709.
- Xiao DL, Xi JW. Efficacy of peripheral nerve blocks for pain management in patients with rib fractures: A systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 2023;27:899-910.
- McKendy KM, Lee LF, Boulva K, Deckelbaum DL, Mulder DS, Razek TS, et al. Epidural analgesia for traumatic rib fractures is associated with worse outcomes: a matched analysis. J Surg Res. 2017;214:117-23.
- Ge YY, Wang XZ, Yuan N, Yuan LY, Ma WH, Hu Y. [Effect of ultrasound guided patient-controlled paravertebral block on pulmonary function in patients with multiple fractured ribs]. Zhonghua Wai Ke Za Zhi. 2016;54:924-8.
- Yeying G, Liyong Y, Yuebo C, Yu Z, Guangao Y, Weihu M, et al. Thoracic paravertebral block versus intravenous patient-controlled analgesia for pain treatment in patients with multiple rib fractures. J Int Med Res. 2017;45:2085-91.
- Jiang M, Peri V, Ou Yang B, Chang J, Hacking D. Erector Spinae Plane Block as an Analgesic Intervention in Acute Rib Fractures: A Scoping Review. Local Reg Anesth. 2023;16:81-90.
- Elawamy A, Morsy MR, Ahmed MAY. Comparison of Thoracic Erector Spinae Plane Block With Thoracic Paravertebral Block for Pain Management in Patients With Unilateral Multiple Fractured Ribs. Pain Physician. 2022;25:483-90.
- Armin E, Movahedi M, Najafzadeh MJ, Honarmand A, Rukerd MRZ, Mirafzal A. COMPARISON OF ULTRASOUND-GUIDED ERECTOR SPINAE PLANE BLOCK WITH INTERCOSTAL NERVE BLOCK FOR TRAUMA-ASSOCIATED CHEST WALL PAIN. J Emerg Med. 2022;63:520-7.
- El Malla DA, Helal RAEF, Zidan TAM, El Mourad MB. The Effect of Erector Spinae Block versus Serratus Plane Block on Pain Scores and Diaphragmatic Excursion in Multiple Rib Fractures. A Prospective Randomized Trial. Pain Med. 2022;23:448-55.
- Partyka C, Asha S, Berry M, Ferguson I, Burns B, Tsacalos K, et al. Serratus Anterior Plane Blocks for Early Rib Fracture Pain Management: The SABRE Randomized Clinical Trial. JAMA Surg. 2024;159:810-7.
- Wallen TE, Singer KE, Makley AT, Athota KP, Janowak CF, Hanseman D, et al. Intercostal liposomal bupivacaine injection for rib fractures: A prospective randomized controlled trial. J Trauma Acute Care Surg. 2022;92:266-76.
- Proaño-Zamudio JA, Argandykov D, Renne A, Gebran A, Ouwerkerk JJJ, Dorken-Gallastegi A, et al. Timing of regional analgesia in elderly patients with blunt chest-wall injury. Surgery. 2023;174:901-6.
- Alizai Q, Arif MS, Colosimo C, Hosseinpour H, Spencer AL, Bhogadi SK, et al. Beyond the short-term relief: Outcomes of geriatric rib fracture patients receiving paravertebral nerve blocks and epidural analgesia. Injury. 2024;55:111184.
- Mukherjee K, Schubl SD, Tominaga G, Cantrell S, Kim B, Haines KL, et al. Non-surgical management and analgesia strategies for older adults with multiple rib fractures: A systematic review, meta-analysis, and joint practice management guideline from the Eastern Association for the Surgery of Trauma and the Chest Wall Injury Society. J Trauma Acute Care Surg. 2023;94:398-407.
- Wunsch H, Gershengorn HB, Cooke CR, Guerra C, Angus DC, Rowe JW, et al. Use of Intensive Care Services for Medicare Beneficiaries Undergoing Major Surgical Procedures. Anesthesiology. 2016;124:899-907.
- Abebe K, Negasa T, Argaw F. Surgical Admissions and Treatment Outcomes at a Tertiary Hospital Intensive Care Unit in Ethiopia: A Two-Year Review. Ethiop J Health Sci. 2020;30:725-32.
- Ranjeva S, Khoudary A, Kaafarani H, Prout L, Nagrebetsky A, Deng H. 123: Postoperative pain in the ICU: A retrospective cohort study on severity and frequency of assessment. Crit Care Med. 2023 Jan;51(1):44–44.
- Mathew A, Lukachan GA, Varughese D, Raju N, Mathai AS, Johnson AS. Impact of frailty and comorbidity index on postoperative complications and functional outcomes among elderly patients undergoing hip fracture surgeries under regional anesthesia techniques. Anaesth Pain Intensive Care. 2023 Apr 25;27(2):161–9.
- Thompson A, Fleischmann KE, Smilowitz NR, de Las Fuentes L, Mukherjee D, Aggarwal NR, et al. 2024 AHA/ACC/ACS/ASNC/HRS/SCA/SCCT/SCMR/SVM Guideline for Perioperative Cardiovascular Management for Noncardiac Surgery: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2024;150:e351-e442.
- Guay J, Kopp S. Peripheral nerve blocks for hip fractures in adults. Cochrane Database Syst Rev. 2020;11:CD001159.
- Laumonerie P, Dalmas Y, Tibbo ME, Robert S, Durant T, Caste T, et al. Sensory Innervation of the Hip Joint and Referred Pain: A Systematic Review of the Literature. Pain Med. 2021;22:1149-57.
- Morrison RS, Dickman E, Hwang U, Akhtar S, Ferguson T, Huang J, et al. Regional Nerve Blocks Improve Pain and Functional Outcomes in Hip Fracture: A Randomized Controlled Trial. J Am Geriatr Soc. 2016;64:2433-9.
- Wan HY, Li SY, Ji W, Yu B, Jiang N. Fascia Iliaca Compartment Block for Perioperative Pain Management of Geriatric Patients with Hip Fractures: A Systematic Review of Randomized Controlled Trials. Pain Res Manag. 2020;2020:8503963.
- Del Buono R, Padua E, Pascarella G, Soare CG, Barbara E. Continuous PENG block for hip fracture: a case series. Reg Anesth Pain Med. 2020;45:835-8.
- Acharya U, Lamsal R. Pericapsular Nerve Group Block: An Excellent Option for Analgesia for Positional Pain in Hip Fractures. Case Rep Anesthesiol. 2020;2020:1830136.
- Lin DY, Morrison C, Brown B, Saies AA, Pawar R, Vermeulen M, et al. Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: a single-center double-blinded randomized comparative trial. Reg Anesth Pain Med. 2021;46:398-403.
- Mosaffa F, Taheri M, Manafi Rasi A, Samadpour H, Memary E, Mirkheshti A. Comparison of pericapsular nerve group (PENG) block with fascia iliaca compartment block (FICB) for pain control in hip fractures: A double-blind prospective randomized controlled clinical trial. Orthop Traumatol Surg Res. 2022;108:103135.
- Desai DJ, Shah N, Bumiya P. Combining Pericapsular Nerve Group (PENG) Block With the Supra-Inguinal Fascia Iliaca Block (SIFICB) for Perioperative Analgesia and Functional Recovery in Patients Undergoing Hip Surgeries: A Retrospective Case Series. Cureus. 2023;15:e36374.
- Dangle J, Kukreja P, Kalagara H. Review of current practices of peripheral nerve blocks for hip fracture and surgery. Curr Anesthesiol Rep. 2020;10:259–66.
- Cunningham DJ, LaRose MA, Zhang GX, Au S, MacAlpine EM, Paniagua AR, et al. Regional anesthesia reduces inpatient and outpatient perioperative opioid demand in periarticular elbow surgery. J Shoulder Elbow Surg. 2022;31:e48-e57.
- Cunningham DJ, LaRose M, Zhang G, Patel P, Paniagua A, Gadsden J, et al. Regional Anesthesia Associated With Decreased Inpatient and Outpatient Opioid Demand in Tibial Plateau Fracture Surgery. Anesth Analg. 2022;134:1072-81.
- Lantieri MA, Novicoff WM, Yarboro SR. Regional anesthesia provides limited decreases in opioid use following distal tibia and ankle fracture surgery. Eur J Orthop Surg Traumatol. 2023;33:2633–8.
- Lee CCM, Beh ZY, Lua CB, Peng K, Fathil SM, Hou JD, Lin JA. Regional Anesthetic and Analgesic Techniques for Clavicle Fractures and Clavicle Surgeries: Part 1-A Scoping Review. Healthcare (Basel). 2022;10:1487.
- Neal JM, Gerancher JC, Hebl JR, Ilfeld BM, McCartney CJ, Franco CD, Hogan QH. Upper extremity regional anesthesia: essentials of our current understanding, 2008. Reg Anesth Pain Med. 2009;34:134-70.
- Li JW, Songthamwat B, Samy W, Sala-Blanch X, Karmakar MK. Ultrasound-Guided Costoclavicular Brachial Plexus Block: Sonoanatomy, Technique, and Block Dynamics. Reg Anesth Pain Med. 2017;42:233-40.
- Dhir S, Sondekoppam RV, Sharma R, Ganapathy S, Athwal GS. A Comparison of Combined Suprascapular and Axillary Nerve Blocks to Interscalene Nerve Block for Analgesia in Arthroscopic Shoulder Surgery: An Equivalence Study. Reg Anesth Pain Med. 2016;41:564-71.
- Akesen S, Akesen B, Atıcı T, Gurbet A, Ermutlu C, Özyalçın A. Comparison of efficacy between the genicular nerve block and the popliteal artery and the capsule of the posterior knee (IPACK) block for total knee replacement surgery: A prospective randomized controlled study. Acta Orthop Traumatol Turc. 2021;55:134-40.
- Chan E, Howle R, Onwochei D, Desai N. Infiltration between the popliteal artery and the capsule of the knee (IPACK) block in knee surgery: a narrative review. Reg Anesth Pain Med. 2021;46:784-805.
- Kang C, Hwang DS, Song JH, Lee GS, Lee JK, Hwang SJ, et al. Clinical analyses of ultrasound-guided nerve block in lower-extremity surgery: A retrospective study. J Orthop Surg (Hong Kong). 2021;29:2309499021989102.
- von Keudell AG, Weaver MJ, Appleton PT, Bae DS, Dyer GSM, Heng M, et al. Diagnosis and treatment of acute extremity compartment syndrome. Lancet. 2015;386:1299–310.
- Driscoll EB, Maleki AH, Jahromi L, Hermecz BN, Nelson LE, Vetter IL, et al. Regional anesthesia or patient-controlled analgesia and compartment syndrome in orthopedic surgical procedures: a systematic review. Local Reg Anesth. 2016;9:65–81.
- Tran AA, Lee D, Fassihi SC, Smith E, Lee R, Siram G. A systematic review of the effect of regional anesthesia on diagnosis and management of acute compartment syndrome in long bone fractures. Eur J Trauma Emerg Surg. 2020;46:1281–90.
- Chen Y-YK, Lirk P, Flowers KM, Colebaugh CA, Wilson JM, Zeballos J, et al. Impact of varying degrees of peripheral nerve blockade on experimental pressure and ischemic pain: adductor canal and sciatic nerve blocks in a human model of compartment syndrome pain. Reg Anesth Pain Med. 2022;47:630–6.
- Ivani G, Suresh S, Ecoffey C, Bosenberg A, Lonnqvist P-A, Krane E, et al. The European Society of Regional Anaesthesia and Pain Therapy and the American Society of Regional Anesthesia and Pain Medicine joint committee practice advisory on controversial topics in pediatric Regional Anesthesia. Reg Anesth Pain Med. 2015;40:526–32.
- Yuan B, Hu D, Gu S, Xiao S, Song F. The global burden of traumatic amputation in 204 countries and territories. Front Public Health. 2023;11:1258853.
- Limakatso K, Bedwell GJ, Madden VJ, Parker R. The prevalence and risk factors for phantom limb pain in people with amputations: A systematic review and meta-analysis. PLoS One. 2020;15:e0240431.
- Birbaumer N, Lutzenberger W, Montoya P, Larbig W, Unertl K, Töpfner S, et al. Effects of regional anesthesia on phantom limb pain are mirrored in changes in cortical reorganization. J Neurosci. 1997;17:5503–8.
- Kukreja P, Paul LM, Sellers AR, Nagi P, Kalagara H. The role of regional anesthesia in the development of chronic pain: A review of literature. Curr Anesthesiol Rep. 2022;12:417–38.
- Ilfeld BM, Khatibi B, Maheshwari K, Madison S, Ali Sakr Esa W, Mariano ER, et al. Patient-centered results from a multicenter study of continuous peripheral nerve blocks and postamputation phantom and residual limb pain: secondary outcomes from a randomized, clinical trial. Reg Anesth Pain Med. 2023;48:471–7.
- Sengupta S. Post-operative pulmonary complications after thoracotomy. Indian J Anaesth. 2015;59:618–26.
- Visser E, Marsman M, van Rossum PSN, Cheong E, Al-Naimi K, van Klei WA, et al. Postoperative pain management after esophagectomy: a systematic review and meta-analysis. Dis Esophagus. 2017;30:1–11.
- Odor PM, Bampoe S, Gilhooly D, Creagh-Brown B, Moonesinghe SR. Perioperative interventions for prevention of postoperative pulmonary complications: systematic review and meta-analysis. BMJ. 2020;368:m540.
- Macrosson D, Beebeejaun A, Odor PM. A systematic review and meta-analysis of thoracic epidural analgesia versus other analgesic techniques in patients post-oesophagectomy. Perioper Med (Lond). 2024;13:80.
- Weinstein EJ, Levene JL, Cohen MS, Andreae DA, Chao JY, Johnson M, et al. Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children. Cochrane Database Syst Rev. 2018;4:CD007105.
- Balzani E, Rosboch GL, Ceraolo E, Lyberis P, Filippini C, Piccioni F, et al. The effect of peripheral regional analgesia in thoracic surgery: a systematic review and a meta-analysis of randomized-controlled trials. Tumori. 2023;109:6–18.
- Yeung JHY, Gates S, Naidu BV, Wilson MJA, Gao Smith F. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016;2:CD009121.
- Ding X, Jin S, Niu X, Ren H, Fu S, Li Q. A comparison of the analgesia efficacy and side effects of paravertebral compared with epidural blockade for thoracotomy: an updated meta-analysis. PLoS One. 2014;9:e96233.
- Baidya DK, Khanna P, Maitra S. Analgesic efficacy and safety of thoracic paravertebral and epidural analgesia for thoracic surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2014;18:626–35.
- Xiong C, Han C, Zhao D, Peng W, Xu D, Lan Z. Postoperative analgesic effects of paravertebral block versus erector spinae plane block for thoracic and breast surgery: A meta-analysis. PLoS One. 2021;16:e0256611.
- Koo C-H, Lee H-T, Na H-S, Ryu J-H, Shin H-J. Efficacy of erector spinae plane block for analgesia in thoracic surgery: A systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2022;36:1387–95.
- Huang W, Wang W, Xie W, Chen Z, Liu Y. Erector spinae plane block for postoperative analgesia in breast and thoracic surgery: A systematic review and meta-analysis. J Clin Anesth. 2020;66:109900.
- Guerra-Londono CE, Privorotskiy A, Cozowicz C, Hicklen RS, Memtsoudis SG, Mariano ER, et al. Assessment of intercostal nerve block analgesia for thoracic surgery: A systematic review and meta-analysis: A systematic review and meta-analysis. JAMA Netw Open. 2021;4:e2133394.
- Lusianawati, Suhardi CJ, Sumartono C, Wungu CDK. Efficacy and safety of the serratus anterior block compared to thoracic epidural analgesia in surgery: Systematic review and meta-analysis. Tzu Chi Med J. 2023;35:329–37.
- Liu X, Song T, Xu H-Y, Chen X, Yin P, Zhang J. The serratus anterior plane block for analgesia after thoracic surgery: A meta-analysis of randomized controlled trails. Medicine (Baltimore). 2020;99:e20286.
- Jack JM, McLellan E, Versyck B, Englesakis MF, Chin KJ. The role of serratus anterior plane and pectoral nerves blocks in cardiac surgery, thoracic surgery and trauma: a qualitative systematic review. Anaesthesia. 2020;75:1372–85.
- McLean SR, von Homeyer P, Cheng A, Hall ML, Mulligan MS, Cain K, et al. Assessing the benefits of preoperative thoracic epidural placement for lung transplantation. J Cardiothorac Vasc Anesth. 2018;32:2654–61.
- Garcia JP, Ashworth CL, Hage CA. ECMO in lung transplant: pre, intra and post-operative utilization—a narrative review. Curr Chall Thorac Surg. 2022;0:0–0.
- Lenz N, Hirschburger M, Roehrig R, Menges T, Mueller M, Padberg W, et al. Application of continuous wound-infusion catheters in lung transplantation: A retrospective data analysis. Thorac Cardiovasc Surg. 2017;65:403–9.
- Hutchins J, Apostolidou I, Shumway S, Kelly R, Wang Q, Foster C, et al. Paravertebral catheter use for postoperative pain control in patients after lung transplant surgery: A prospective observational study. J Cardiothorac Vasc Anesth. 2017;31:142–6.
- Rigg JRA, Jamrozik K, Myles PS, Silbert BS, Peyton PJ, Parsons RW, et al. Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet. 2002;359:1276–82.
- Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis: A meta-analysis. JAMA. 2003;290:2455–63.
- Carver A, Wou F, Pawa A. Do outcomes differ between thoracic epidurals and continuous fascial plane blocks in adults undergoing major abdominal surgery? Curr Anesthesiol Rep. 2023;14:25–41.
- Bardia A, Sood A, Mahmood F, Orhurhu V, Mueller A, Montealegre-Gallegos M, et al. Combined epidural-general anesthesia vs general anesthesia alone for elective abdominal aortic aneurysm repair. JAMA Surg. 2016;151:1116–23.
- Monaco F, Pieri M, Barucco G, Karpatri V, Redaelli MB, De Luca M, et al. Epidural analgesia in open thoraco-abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg. 2019;57:360–7.
- Guay J, Kopp S. Epidural pain relief versus systemic opioid-based pain relief for abdominal aortic surgery. Cochrane Database Syst Rev. 2016;2017:CD005059.
- Greco KJ, Brovman EY, Nguyen LL, Urman RD. The impact of epidural analgesia on perioperative morbidity or mortality after open abdominal aortic aneurysm repair. Ann Vasc Surg. 2020;66:44–53.
- Hermanides J, Hollmann MW, Stevens MF, Lirk P. Failed epidural: causes and management. Br J Anaesth. 2012;109:144–54.
- Holte K, Foss NB, Svensén C, Lund C, Madsen JL, Kehlet H. Epidural anesthesia, hypotension, and changes in intravascular volume. Anesthesiology. 2004;100:281–6.
- Jackson CB, Desai J, Lee WA, Renfro LA. Utility of continuous paravertebral block after retroperitoneal abdominal aortic aneurysm repair. Ann Vasc Surg. 2024;104:124–31.
- Minami K, Yoshitani K, Inatomi Y, Sugiyama Y, Iida H, Ohnishi Y. A retrospective examination of the efficacy of paravertebral block for patients requiring intraoperative high-dose unfractionated heparin administration during thoracoabdominal aortic aneurysm repair. J Cardiothorac Vasc Anesth. 2015;29:937–41.
- Walker C, Carneiro J, Bersot CDA, Barros V, Aslanidis T. Unilateral erector spinae plane block as adjuvant for open repair of thoracoabdominal aortic aneurysm: Case report and literature review [Internet]. 2023. Available from: https://rgdoi.net/10.13140/RG.2.2.20265.98400
- Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus lumborum block: Anatomical concepts, mechanisms, and techniques. Anesthesiology. 2019;130:322–35.
- Tran DQ, Bravo D, Leurcharusmee P, Neal JM. Transversus Abdominis Plane Block: A Narrative Review. Anesthesiology. 2019;131:1166-90.
- Feltracco P, Carollo C, Barbieri S, Milevoj M, Pettenuzzo T, Gringeri E, et al. Pain control after liver transplantation surgery. Transplant Proc. 2014;46:2300–7.
- Hausken J, Haugaa H, Hagness M, Line P-D, Melum E, Tønnessen TI. Thoracic epidural analgesia for postoperative pain management in liver transplantation: A 10-year study on 685 liver transplant recipients: A 10-year study on 685 liver transplant recipients. Transplant Direct. 2021;7:e648.
- Dieu A, Huynen P, Lavand’homme P, Beloeil H, Freys SM, Pogatzki-Zahn EM, et al. Pain management after open liver resection: Procedure-Specific Postoperative Pain Management (PROSPECT) recommendations. Reg Anesth Pain Med. 2021;46:433–45.
- Ander M, Mugve N, Crouch C, Kassel C, Fukazawa K, Isaak R, et al. Regional anesthesia for transplantation surgery - A White Paper Part 2: Abdominal transplantation surgery. Clin Transplant. 2024;38:e15227.
- Guay J, Kopp S. Epidural analgesia for adults undergoing cardiac surgery with or without cardiopulmonary bypass. Cochrane Database Syst Rev. 2019;3:CD006715.
- Ho AM, Chung DC, Joynt GM. Neuraxial blockade and hematoma in cardiac surgery: estimating the risk of a rare adverse event that has not (yet) occurred. Chest. 2000;117:551–5.
- Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American society of regional anesthesia and pain medicine evidence-based guidelines (fourth edition). Reg Anesth Pain Med. 2018;43:263–309.
- Devarajan J, Balasubramanian S, Nazarnia S, Lin C, Subramaniam K. Regional Analgesia for Cardiac Surgery Part 1. Current status of neuraxial and paravertebral blocks for adult cardiac surgery. Semin Cardiothorac Vasc Anesth. 2021;25:252–64.
- Naganuma M, Tokita T, Sato Y, Kasai T, Kudo Y, Suzuki N, et al. Efficacy of preoperative bilateral thoracic paravertebral block in cardiac surgery requiring full heparinization: A propensity-matched study. J Cardiothorac Vasc Anesth. 2022;36:477–82.
- Scarfe AJ, Schuhmann-Hingel S, Duncan JK, Ma N, Atukorale YN, Cameron AL. Continuous paravertebral block for post-cardiothoracic surgery analgesia: a systematic review and meta-analysis. Eur J Cardiothorac Surg. 2016;50:1010–8.
- Höhener D, Blumenthal S, Borgeat A. Sedation and regional anaesthesia in the adult patient. Br J Anaesth. 2008;100:8–16.
- Elsharkawy H, Pawa A, Mariano ER. Interfascial plane blocks: Back to basics. Reg Anesth Pain Med. 2018;43:341–6.
- Neal JM, Barrington MJ, Brull R, Hadzic A, Hebl JR, Horlocker TT, et al. The second ASRA practice advisory on neurologic complications associated with regional anesthesia and pain medicine: Executive summary 2015. Reg Anesth Pain Med. 2015;40:401–30.
- Topor B, Oldman M, Nicholls B. Best practices for safety and quality in peripheral regional anaesthesia. BJA Educ. 2020;20:341–7.
- Walker BJ, Long JB, Sathyamoorthy M, Birstler J, Wolf C, Bosenberg AT, et al. Complications in pediatric regional anesthesia: An analysis of more than 100,000 blocks from the Pediatric Regional Anesthesia Network: An analysis of more than 100,000 blocks from the pediatric regional anesthesia network. Anesthesiology. 2018;129:721–32.
- Ramin S, Bringuier S, Martinez O, Sadek M, Manzanera J, Deras P, et al. Continuous peripheral nerve blocks for analgesia of ventilated critically ill patients with multiple trauma: a prospective randomized study. Anaesth Crit Care Pain Med. 2023;42:101183.
- Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP, et al. Clinical Practice Guidelines for the prevention and management of Pain, Agitation/sedation, Delirium, Immobility, and Sleep disruption in Adult Patients in the ICU. Crit Care Med. 2018;46:e825–73.
- Vincent J-L, Sakr Y, Singer M, Martin-Loeches I, Machado FR, Marshall JC, et al. Prevalence and outcomes of infection among patients in intensive care units in 2017. JAMA. 2020;323:1478–87.
- Selvamani BJ, Kalagara H, Volk T, Narouze S, Childs C, Patel A, et al. Infectious complications following regional anesthesia: a narrative review and contemporary estimates of risk. Reg Anesth Pain Med. 2024;rapm-2024-105496.
- Rasouli MR, Cavanaugh PK, Restrepo C, Ceylan HH, Maltenfort MG, Viscusi ER, et al. Is neuraxial anesthesia safe in patients undergoing surgery for treatment of periprosthetic joint infection? Clin Orthop Relat Res. 2015;473:1472–7.
- Neuburger M, Büttner J, Blumenthal S, Breitbarth J, Borgeat A. Inflammation and infection complications of 2285 perineural catheters: a prospective study. Acta Anaesthesiol Scand. 2007;51:108–14.
- Capdevila X, Pirat P, Bringuier S, Gaertner E, Singelyn F, Bernard N, et al. Continuous peripheral nerve blocks in hospital wards after orthopedic surgery: a multicenter prospective analysis of the quality of postoperative analgesia and complications in 1,416 patients. Anesthesiology. 2005;103:1035–45.
- Morin AM, Kerwat KM, Klotz M, Niestolik R, Ruf VE, Wulf H, et al. Risk factors for bacterial catheter colonization in regional anaesthesia. BMC Anesthesiol. 2005;5:1.
- Bomberg H, Kubulus C, Herberger S, Wagenpfeil S, Kessler P, Steinfeldt T, et al. Tunnelling of thoracic epidural catheters is associated with fewer catheter-related infections: a retrospective registry analysis. Br J Anaesth. 2016;116:546–53.
- Schmoch T, Möhnle P, Weigand MA, Briegel J, Bauer M, Bloos F, et al. The prevalence of sepsis-induced coagulopathy in patients with sepsis - a secondary analysis of two German multicenter randomized controlled trials. Ann Intensive Care. 2023;13:3.
- Derakhshanfar H, Vafaei A, Tabatabaey A, Noori S. Prevalence and associated factors of acute traumatic coagulopathy; A cross sectional study. Emerg (Tehran). 2017;5:e58.
- Kietaibl S, Ferrandis R, Godier A, Llau J, Lobo C, Macfarlane A Jr, et al. Regional anaesthesia in patients on antithrombotic drugs: Joint ESAIC/ESRA guidelines: Joint ESAIC/ESRA guidelines. Eur J Anaesthesiol. 2022;39:100–32.
- Joubert F, Gillois P, Bouaziz H, Marret E, Iohom G, Albaladejo P. Bleeding complications following peripheral regional anaesthesia in patients treated with anticoagulants or antiplatelet agents: A systematic review. Anaesth Crit Care Pain Med. 2019;38:507–16.
- Working Party:; Association of Anaesthetists of Great Britain & Ireland; Obstetric Anaesthetists’ Association; Regional Anaesthesia UK. Regional anaesthesia and patients with abnormalities of coagulation: the Association of Anaesthetists of Great Britain & Ireland The Obstetric Anaesthetists’ Association Regional Anaesthesia UK. Anaesthesia. 2013;68:966-72.
- Arbona FL, Khabiri B, Norton JA. Ultrasound-Guided Regional Anesthesia: A Practical Approach to Peripheral Nerve Blocks and Perineural Catheters. Cambridge University Press; 2011. 207 p.
- Dung-Hung C, Cong T, Zeyu J, Yu-Shan OY, Yung-Yan L. External validation of a machine learning model to predict hemodynamic instability in intensive care unit. Crit Care. 2022;26:215.
- Meyhoff CS, Hesselbjerg L, Koscielniak-Nielsen Z, Rasmussen LS. Biphasic cardiac output changes during onset of spinal anaesthesia in elderly patients. Eur J Anaesthesiol. 2007;24:770-5.
- Wink J, Veering BT, Aarts LPHJ, Wouters PF. Effects of thoracic epidural anesthesia on neuronal cardiac regulation and cardiac function. Anesthesiology. 2019;130:472–91.
- Scott DA, Beilby DS, McClymont C. Postoperative analgesia using epidural infusions of fentanyl with bupivacaine. A prospective analysis of 1,014 patients. Anesthesiology. 1995;83:727-37.
- Eichenberger U, Giani C, Petersen-Felix S, Graven-Nielsen T, Arendt-Nielsen L, Curatolo M. Lumbar epidural fentanyl: segmental spread and effect on temporal summation and muscle pain. Br J Anaesth. 2003;90:467-73.
- Mohta M, Verma P, Saxena AK, Sethi AK, Tyagi A, Girotra G. Prospective, randomized comparison of continuous thoracic epidural and thoracic paravertebral infusion in patients with unilateral multiple fractured ribs--a pilot study. J Trauma. 2009;66:1096-101.
- Frölich MA, Arabshahi A, Katholi C, Prasain J, Barnes S. Hemodynamic characteristics of midazolam, propofol, and dexmedetomidine in healthy volunteers. J Clin Anesth. 2011;23:218-23.
- Tikle HA, Patil BM. Comparison of superficial cervical plexus block versus local infiltration for pain relief during internal jugular vein cannulation. Int J Contemp Med Res [IJCMR] [Internet]. 2018 Sep;5(9).
- Lopez-Rincon RM, Kumar V. Ultrasound-guided intercostal nerve block. 2020; Available from: https://www.ncbi.nlm.nih.gov/books/NBK555900/
Copyright and license
Copyright © 2024 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.